If you’ve lived for any length of time with a form of arthropathy, then you can attest to the aching, burning, gnawing, and piercing pain that attacks your joints. Maybe it’s just one joint, maybe multiple, but no matter what, arthritis is an incredibly debilitating condition. Arthropathy refers to any kind of disease of the joints. The main types of arthropathy are forms of arthritis, which is an inflammation of the joints. Unfortunately, most forms of arthropathy can’t be cured — some are autoimmune, and sometimes the amount of damage done to joints can be reversed. However, just because a condition might not be reversible or preventable doesn't mean it isn’t treatable. Let’s look at some common types of arthropathies and ways to relieve the symptoms they cause.
What Are the Different Types of Arthropathies?
 Most of the major forms of arthropathies are forms of inflammatory arthritis. Any “-itis” is an inflammatory condition where the joint has been damaged or agitated. There are some diseases and conditions that mimic the type of pain you experience when you have arthritis, and this can cause some confusion. Let’s take a look at some of these conditions: Most of the major forms of arthropathies are forms of inflammatory arthritis. Any “-itis” is an inflammatory condition where the joint has been damaged or agitated. There are some diseases and conditions that mimic the type of pain you experience when you have arthritis, and this can cause some confusion. Let’s take a look at some of these conditions:
Osteoarthritis
The most common form of arthritis, osteoarthritis, usually affects those who are above the age of 50. If there’s a lot of wear and tear on particular joints in your body, you’re typically at a higher risk of developing osteoarthritis. It may be in just one joint or affect multiple. Common physical reasons for developing osteoarthritis include:
-
Running: Because of the constant pounding on the knee joints, runners do have a higher risk of developing arthritis in their knees.
-
Typing: Long hours of pressing your fingers down can wear out the finger and wrist joints and cause inflammation.
-
Manual labor: Any job involving heavy lifting or moving large items carries an increased risk of developing osteoarthritis.
When you have osteoarthritis, it feels like your joints are burning, aching, sore, or tender, but it can also cause sharp pains with certain movements.
Rheumatoid Arthritis (RA)
RA is different from osteoarthritis because it’s an autoimmune condition, so the body itself causes damage to the affected joints. Specifically, RA attacks the lining of the joints, causing painful inflammation that can eventually even wear down the bones. It’s common to experience morning stiffness, soreness after using certain joints, and sometimes even sudden attacks of sharp pain. Other risk factors include age (you’re more likely to develop RA if you’re older) and sex (women are more prone to RA than men).
Psoriatic Arthritis
About 10% of people who develop psoriasis, a painful form of skin inflammation, will also develop psoriatic arthritis. This type of arthritis causes swelling in the joints, usually targeting the fingers, toes, and lower back. It doesn’t usually affect the number of joints that RA does, but like RA, it’s not known to be curable, so treatment is about managing symptoms and flare-ups.
Gout (Metabolic Arthritis) and Pseudogout
Gout is a form of arthritis caused by a buildup of uric acid in the joints. The acid is then crystallized and causes the joints to become inflamed. It usually affects the big toe and, unlike other forms of arthritis, doesn’t come on slowly, but suddenly and often violently in small joints like the fingers and toes. A related condition is pseudogout, which is similar to gout but results from a buildup of calcium in the joints and usually affects the knee. Both gout and pseudogout cause swelling, tenderness, and intense pain.
Ankylosing Spondylitis
This autoimmune form of arthritis can be fairly serious and tends to affect men more than women, usually under 30. Ankylosing spondylitis attacks the ligaments and tendons that join bones, especially around the spine and pelvis. Eventually, the disease can lead to the spinal vertebrae fusing together and becoming completely stiff.
Spondyloarthritis
Spondyloarthritis is a form of inflammatory arthritis that affects the spine and causes lower back pain. Sometimes it can also affect the arms and legs as well. Although it doesn’t have a cure, it can be managed with medication and exercise.
Arthopathic-Like Conditions
Some autoimmune diseases and neuropathic conditions can cause pain, numbness, tingling, and strange sensations, often in the joints. Some of these disorders include:
-
Lupus: The most common form of lupus is called systemic lupus erythematosus (SLE). This disorder attacks the immune system and causes extreme fatigue, rashes, lesions on the skin, and widespread joint pain.
-
Fibromyalgia: Another autoimmune disorder, fibromyalgia affects the central nervous system and causes severe fatigue, headaches, body aches, and joint pain. There is still a lot to be learned about this disorder, but some of the common symptoms are very similar to forms of arthritis.
-
Neuropathy: Unlike arthritis, neuropathy isn’t caused by inflammation but by damage to the central nervous system through conditions like diabetes or celiac disease. If you have neuropathy, you may feel stinging, burning, freezing, aching, or even electric sensations in your hands and feet.
-
Lyme disease: Usually, a course of doxycycline or a similar antibiotic can cure this tick-borne bacterial infection without any long-term consequences. However, while not specifically a form of arthropathy, lyme, if not caught and treated early, can cause long-term side effects that include constant tiredness, severe brain fog, full body aches, and joint pain.
How Can You Manage Inflammatory Arthritis?
 If you have a form of arthritis that’s already been diagnosed, then much of your focus is going to be on managing your flare-ups and symptoms. There are a number of treatments that can help alleviate the discomfort, but there are also lifestyle patterns that can help to encourage less inflammation in your body, as well as more mobility and range of motion in the joints. If you have a form of arthritis that’s already been diagnosed, then much of your focus is going to be on managing your flare-ups and symptoms. There are a number of treatments that can help alleviate the discomfort, but there are also lifestyle patterns that can help to encourage less inflammation in your body, as well as more mobility and range of motion in the joints.
Medical Treatments
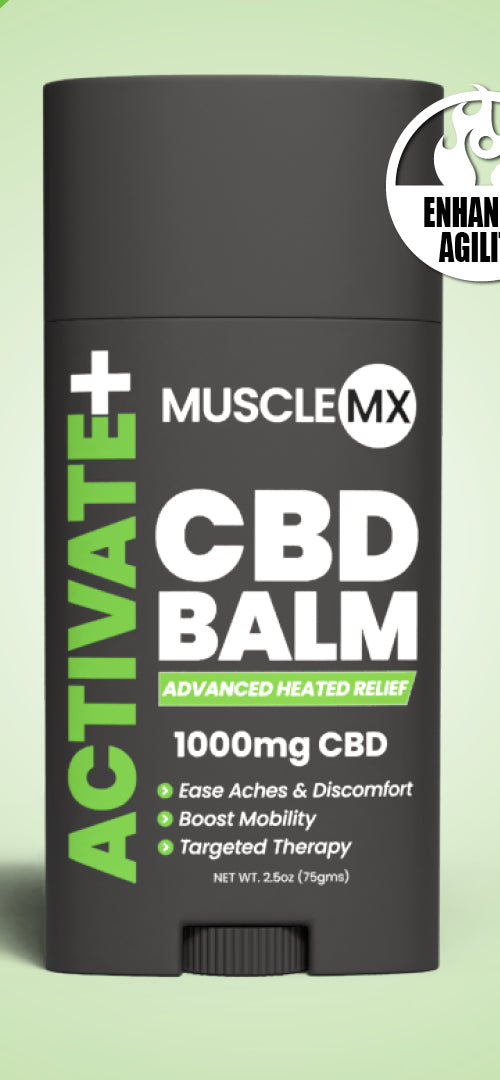
Inflammatory arthritis may be relieved through the use of certain medications or interventions. Here are some of the common treatment options: Topicals There are many balms, creams, lotions, and oils that can be applied to areas that are experiencing discomfort from arthritis. These are often medicines in a topical form, like lidocaine (which numbs the area from pain) or NSAIDs (non-steroidal anti-inflammatory drugs). There are also many natural, herbal, and plant-based topicals that can work to soothe feelings of tension or confuse the nerves to distract from pain (for example, balms made from hot chili peppers). Physical Therapy You can improve movement and mobility in specific areas of the body with physical therapy. You can work with a physical therapist for a few weeks, a few months, or even an extended period of time, depending on your needs. Physical therapists can often teach you exercises you can do at home to strengthen the muscles around your joints. Medication A wide variety of medications and supplements are available to alleviate pain and inflammation from arthritis. NSAIDs, like ibuprofen, can be used to lessen inflammation. A doctor can prescribe prescription pain relievers and muscle relaxers for more severe symptoms. In some cases, a doctor may prescribe antidepressants or medication for nerve pain. Injections Several types of injections can help with arthritis pain if medication or physical therapy isn’t sufficient. Hyaluronic acid is a synthetic liquid injected in a joint that’s very similar to the fluid that naturally lubricates them. If you have severe osteoarthritis, this is an option. Corticosteroid injections put steroids into the joint that can help relieve intense pain. Surgical Procedures In more serious inflammatory diseases, surgery may be necessary. If a joint has deteriorated due to an arthritis disease, a joint replacement might be necessary. This procedure involves the surgical removal of the joint and the replacement with a plastic or metal joint.
Lifestyle Factors
Lifestyle changes can also influence arthritic symptoms. From your physical activity to your weight to your diet and stress management, your lifestyle choices significantly impact your overall wellness. Here is an overview of a few lifestyle choices that may help you manage inflammatory arthritis: Maintain a Healthy Weight Because excess weight can put more strain on joints (especially the knees), trying to stay at a healthy weight is important. Proper diet and exercise can help make the weight loss process go quicker, allowing you to experience some relief from some arthritis symptoms faster. Stretching Exercises A physical therapist, chiropractor, or sports medicine professional can offer great tips on stretches that will improve your mobility and range of motion in your joints. If there’s a specific problem area, a good stretching routine can strengthen your muscles so that there’s less strain on your joints. Stay Active Exercising is important because it maintains your ability to get around and do daily tasks and because a healthy heart encourages oxygen flow in the blood. A good supply of oxygen to the joints can help slow joint deterioration from arthritis. Take It Easy Stress can wreak havoc on your overall well-being. Pain that you’re already experiencing can be exacerbated by feeling low, tense, or on edge. Take the necessary steps to deal with your emotional and mental health, and your body will thank you! Get Regular Check-Ups If you have inflammatory arthritis, make sure that you stay on top of it by keeping up with your primary care provider. X-rays, MRIs, blood tests, and a physical examination can give your healthcare provider the information they need to help make suggestions about what would benefit you the most in treating your condition.
Living Your Healthiest Life
No matter what condition you’re struggling with, there is hope to be had for a more comfortable life. While some medical interventions might be necessary, it’s worth making simple lifestyle changes and forming good habits to encourage better body function. If you suspect you might have a form of arthritis, talk to your doctor — early diagnosis makes a difference in treatment. Sources: Arthropathy | Johns Hopkins Medicine Osteoarthritis | OA | MedlinePlus Psoriatic arthritis - Symptoms and causes | Mayo Clinic What Makes Arthritis Flare Up? | Houston Methodist Role of Exercise in Arthritis Management | Johns Hopkins Stress and Arthritis | UW Orthopaedics and Sports Medicine
|






























 Most of the major forms of
Most of the major forms of  If you have a form of arthritis that’s already been diagnosed, then much of your focus is going to be on managing your
If you have a form of arthritis that’s already been diagnosed, then much of your focus is going to be on managing your