What Are the Early Warning Signs of Psoriatic Arthritis?
|
| Are you or someone you know struggling with skin irritation and joint pain? Unfortunately, it may be more than just a coincidence. Psoriatic arthritis is an autoimmune disease affecting millions worldwide, and it can be a life-altering experience. |
This condition occurs when the immune system mistakenly attacks the skin and joints, causing inflammation, pain, and stiffness. For those living with psoriatic arthritis, every day can be a battle, but it's important to remember that you are not alone in this journey.
In this blog, we will dive into psoriatic arthritis and explore the early warning signs, symptoms, and treatment options to help those affected better understand and manage their condition.
What Is Psoriatic Arthritis?
Think of psoriatic arthritis as a partner to psoriasis, a skin condition that causes red, scaly patches. Although the two are connected, they are separate health issues that require particular attention and care. Therefore, understanding the relationship between psoriasis and psoriatic arthritis is crucial in managing this condition effectively.
Living with psoriatic arthritis can feel like navigating a rocky road compared to other forms of arthritis, such as rheumatoid arthritis and osteoarthritis. The pain and stiffness caused by psoriatic arthritis can impact unexpected body parts, like the fingers and toes, and can cause nail changes and eye inflammation.
It's like having a hidden companion that affects daily life. With this condition, both psoriasis and arthritis can flare up and get worse over time.
What Are Some Early Warning Signs of Psoriatic Arthritis?

It's vital to always be on the lookout for the early warning signs of psoriatic arthritis. These red flags can provide essential clues to the condition's onset and help you take control of your health.
Joint Pain
Imagine waking up in the morning with a dull ache in your fingers, toes, or wrists. This persistent joint pain is one of the most common symptoms of psoriatic arthritis and can range from mild discomfort to severe, debilitating pain.
Dactylitis
Dactylitis is a type of swelling that may occur in your fingers or toes, and it can be a tell-tale sign of psoriatic arthritis. However, dactylitis may also indicate other problems, so you should consult your doctor if you suspect you may be dealing with this form of swelling.
Enthesitis
The ligaments and tendons that attach your bones to your muscles can become inflamed in individuals with psoriatic arthritis, a condition known as enthesitis. This can cause pain and tenderness in areas such as the heel or the Achilles tendon.
Skin Symptoms
For individuals with psoriatic arthritis, the skin can also provide early warning signs. Look out for scaly patches, skin lesions, and nail changes such as pitting or depressions in the nail bed. Skin symptoms are like messages sent from your joints to your skin, warning you of the onset of psoriatic arthritis.
Eye Inflammation (Uveitis)
In some cases, psoriatic arthritis can also cause eye inflammation, leading to eye pain, redness, and vision loss. This condition, known as uveitis, can impact an individual's quality of life and daily activities.
What Are Some Precursor Indicators of Psoriatic Arthritis?
Unlocking the mystery of psoriatic arthritis requires a closer examination of the various factors involved, including the immune system's role and potential risk factors. By being mindful of these precursor indicators, individuals can take proactive steps toward managing their condition and preserving their quality of life.
Immune System Involvement
The underlying mechanism of psoriatic arthritis involves the immune system's malfunction, leading to persistent inflammation and pain in the skin and joints. This autoimmune response results from the activation of T-cells, a type of white blood cell, which trigger an inflammatory cascade that leads to the destruction of healthy joint tissue.
The chronic inflammation that results from this immune system malfunction can lead to joint damage, pain, and functional limitations.
Risk Factors
Several risk factors have been associated with an increased likelihood of developing psoriatic arthritis, including a family history of psoriasis or psoriatic arthritis and a personal history of inflammatory bowel disease. Other factors, such as smoking and obesity, have also increased the risk of developing psoriatic arthritis.
Foot Pain, Lower Back Pain, and Reduced Range of Motion
In individuals with psoriatic arthritis, the presence of foot pain, lower back pain, and reduced range of motion can be early indicators of the condition. These symptoms can result from the enthesitis or inflammation of the ligaments and tendons that attach bones to muscles, leading to pain and tenderness in affected areas.
The chronic inflammation associated with psoriatic arthritis can also cause synovitis, or inflammation of the joint lining, leading to joint swelling, pain, and reduced range of motion.
Nail Changes
Do you ever look down at your toenails and see pitting or depressions in the nail bed? This can signify psoriatic arthritis — a red flag that should not be ignored. Other nail changes associated with psoriatic arthritis include discoloration, crumbling nails, and separation of the nail from the nail bed.
How Is Psoriatic Arthritis Diagnosed?
The prompt and accurate diagnosis of psoriatic arthritis is crucial in developing an effective treatment plan and preventing joint damage. Seeking healthcare from a specialist, such as a dermatologist or a rheumatologist, who has expertise in the management of autoimmune diseases, is an essential first step in the diagnostic process.
The following diagnostic tools are commonly used in the evaluation of psoriatic arthritis:
X-Rays
X-rays can provide valuable information about joint damage and swelling. They can reveal the presence of bone erosions, joint space narrowing, and the formation of new bone (known as osteophytes), characteristic of chronic joint inflammation.
Blood Tests
Blood tests can be used to measure markers of inflammation, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), as well as levels of rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies. Elevated levels of these markers can be indicative of the presence of chronic joint inflammation.
Peripheral Joint Swelling Assessment
A peripheral joint swelling assessment is a simple physical examination tool that measures swelling in peripheral joints such as the fingers, toes, wrists, and ankles. The presence of peripheral joint swelling is a hallmark of psoriatic arthritis.
Synovial Fluid Analysis
In some cases, a sample of the fluid within the affected joint (known as synovial fluid) may be collected and analyzed for inflammatory markers. The presence of elevated white blood cells and cytokines levels in the synovial fluid can indicate joint inflammation.
Imaging Studies
In some cases, imaging studies such as magnetic resonance imaging (MRI) or ultrasound may be used to evaluate joint damage and inflammation further. These studies can provide detailed images of the joint tissues that help detect early joint damage and monitor disease progression.
By utilizing various diagnostic tools, healthcare providers can accurately diagnose psoriatic arthritis and develop an effective treatment plan to prevent joint damage and maintain quality of life.
What Are the Treatment Options for Psoriatic Arthritis?
Choosing the right treatment plan for your psoriatic arthritis is key to live a healthier, more comfortable life. Here is a rundown of some common treatment methods for psoriatic arthritis.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and DMARDs
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can manage pain and inflammation in individuals with psoriatic arthritis.
In some cases, disease-modifying antirheumatic drugs (DMARDs), such as methotrexate, may be prescribed to control the immune system's misdirected response and prevent joint damage.
Physical Therapy and Flare-Up Management
Physical therapy can help individuals with psoriatic arthritis maintain flexibility and range of motion and reduce the risk of joint damage. In addition, managing flare-ups, or increased joint pain and inflammation episodes, is an essential component of the overall treatment plan.
This may involve NSAIDs, rest, and other measures to control the immune system's misdirected response and reduce joint inflammation.
Biologic Agents
Biologic agents, such as tumor necrosis factor (TNF) inhibitors, can target specific pathways in the immune system that contribute to joint inflammation and skin symptoms. As a result, these medications can effectively control the immune system's misdirected response and reduce joint inflammation.
Corticosteroids
Corticosteroids, such as prednisone, can reduce joint inflammation and manage symptoms during flare-ups rapidly. However, long-term use of corticosteroids can have significant side effects, and they should be used with caution and under the supervision of a healthcare provider.
Lifestyle Modifications
Lifestyle modifications, such as maintaining a healthy diet and exercise program, can help individuals with psoriatic arthritis maintain their health and manage their symptoms. In addition, stress management techniques, such as meditation and yoga, can help to reduce the impact of stress on the immune system and manage symptoms.
Complementary Therapies
Complementary therapies, such as acupuncture and massage, can manage pain and improve overall well-being in individuals with psoriatic arthritis. However, these therapies should be used in conjunction with conventional medical treatments and under the supervision of a healthcare provider.

How Can Diet Impact Psoriatic Arthritis?
The role of diet in the management of psoriatic arthritis is an area of ongoing research. Studies have shown that specific dietary patterns, such as the Mediterranean diet, can help to reduce inflammatory responses and manage symptoms in individuals with psoriatic arthritis.
Mediterranean Diet
The Mediterranean diet is rich in fruits, vegetables, whole grains, and healthy fats, such as olive oil. It also includes moderate amounts of fish and poultry and limited amounts of red meat and dairy products. This dietary pattern has been shown to reduce inflammation and improve overall health in individuals with psoriatic arthritis.
Anti-Inflammatory Diet
The anti-inflammatory diet is based on the principles of the Mediterranean diet and emphasizes the consumption of foods known to have anti-inflammatory properties. This includes foods rich in omega-3 fatty acids, such as fatty fish, and foods high in antioxidants, such as berries and leafy greens.
Gluten-Free Diet
Some individuals with psoriatic arthritis are sensitive to gluten, a protein in wheat, barley, and rye. Eliminating gluten from the diet has been shown to reduce inflammation and improve symptoms in some individuals with psoriatic arthritis.
Ketogenic Diet
The ketogenic diet may help to reduce inflammation in individuals with psoriatic arthritis by lowering insulin levels and decreasing the production of pro-inflammatory cytokines. Insulin is a hormone that regulates blood sugar levels and is also involved in regulating inflammation.
A high-carbohydrate diet can lead to elevated insulin levels, exacerbating inflammation in individuals with psoriatic arthritis.
On the other hand, a low-carbohydrate diet, such as the ketogenic diet, can reduce insulin levels and decrease the production of pro-inflammatory cytokines. This inflammation reduction can help improve symptoms and prevent joint damage in individuals with psoriatic arthritis.
Fermented Foods
Fermented foods, such as yogurt, kefir, and sauerkraut, contain beneficial bacteria that can help to improve gut health and reduce inflammation. Incorporating fermented foods into the diet can help to manage symptoms in individuals with psoriatic arthritis.
It is important to note that while dietary changes can be beneficial in managing psoriatic arthritis, they should be used in conjunction with conventional medical treatments. In addition, individuals should be mindful of the potential for nutrient deficiencies and take steps to ensure that their diets are balanced and nutritionally adequate.
Key Takeaways
Managing psoriatic arthritis requires an extensive treatment plan and a host of tools to manage the condition. This can include a range of treatment options, such as nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), biologic agents, corticosteroids, and physical therapy.
Diet can also play a role in managing symptoms, with specific dietary patterns, such as the Mediterranean and anti-inflammatory diets, being shown to reduce inflammation and improve overall health.
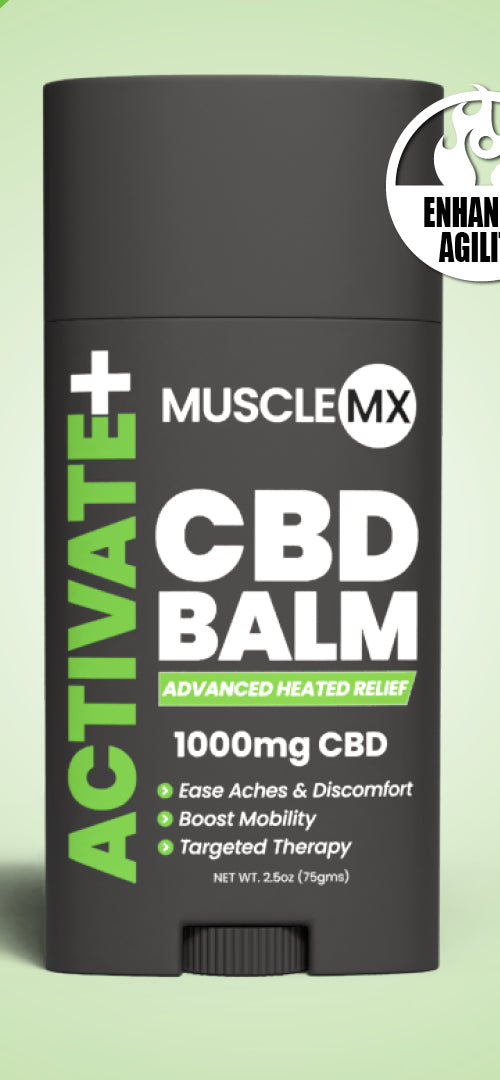
Living with psoriatic arthritis can be a challenging and painful experience, but it doesn't have to be. At Muscle MX, we work to acknowledge the unique needs of individuals with psoriatic arthritis. Join us on the journey to optimal health and unleash your body's full potential with Muscle MX.
Sources:
ESR Information | Mount Sinai
Synovial fluid analysis Information | Mount Sinai
DMARDs | Arthritis Foundation
Cytokines, Inflammation and Pain | PMC