Defining Acute Pain: Understanding Your Pain
|
| Pain is an inevitable aspect of human existence. It’s a protective mechanism designed to alert us of potential harm — yet, it can severely impact one's quality of life when it becomes persistent. |
Acute pain, as opposed to chronic pain, is a sudden and intense sensation caused by a specific event or injury, typically subsiding once the underlying cause is addressed. Despite its temporary nature, acute pain can be debilitating, and can profoundly impact daily activities.
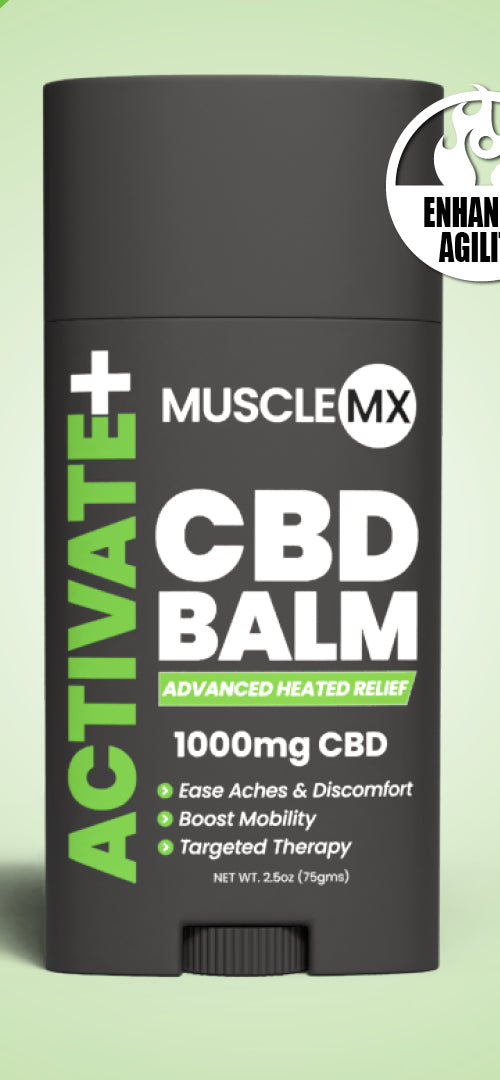
Understanding acute pain is the first step toward managing it. Today, Muscle MX is diving into the intricacies of acute pain, how to manage it, and when it's necessary to seek professional help.
What Is Acute Pain?

There are many different types of pain, each with its unique characteristics and causes. Acute pain comes on suddenly, and many people with acute pain can typically point to an exact trigger that caused the pain.
Here are some of the most common types of acute pain.
Postoperative Pain
This type of acute pain follows surgery, and the intensity can vary depending on the procedure but typically subsides as the body heals.
When an individual experiences pain, their body initiates a complex biological process called nocioception to reduce, and eventually eliminate, the sensation. However, this process can take several days or weeks, which is why it can take a while for postoperative pain to subside.
Acute Injury Pain
Broken bones, sprains, and strains can all cause acute injury pain. This pain is often accompanied by swelling and tenderness but can be relieved with rest, ice, and over-the-counter pain medication such as ibuprofen, acetaminophen, and naproxen.
Neuropathic Pain
Neuropathic pain is caused by nerve damage, either from injury or disease. Neuropathic pain can lead to a variety of sensations, including burning, tingling, sensations of electric shock, or a feeling of numbness.
Neuropathic pain can be challenging to manage and may require more intensive treatment options, such as nerve blocks or medications designed to target the source of the pain.
Fibromyalgia
Fibromyalgia is a chronic condition that can cause widespread pain, tenderness, and fatigue. Although classified as a chronic condition, fibromyalgia can cause sudden and intense episodes of pain that are considered acute.
One of the main difficulties in diagnosing fibromyalgia is the lack of clear biochemical markers. Unlike other medical conditions, no specific test or imaging can diagnose fibromyalgia, making it a complex condition to manage.
Postural Pain
Modern society has shifted to predominately sedentary lifestyles. Poor postures, such as slouching or excessive sitting, can lead to muscle fatigue, altered breathing patterns, neck pain, and lower back pain. Our bodies evolved to move, and when we fail to move regularly, it can eventually lead to pain.
How Is Pain Treated?
Because pain is a complex phenomenon, the management of acute pain requires an integrated and individualized approach. There are several modalities for managing pain, including medications, physical therapy, and complementary and alternative therapies.
Medications
Medications play a crucial role in managing pain. There is a wide range of options available, including analgesics, anti-inflammatory drugs, anesthetics, and other pain relief options.
Analgesics, such as non-steroidal anti-inflammatory drugs (NSAIDs), are the cornerstones of pain management. These medications work to block pain signals from reaching the brain, relieving moderate to severe pain.
Anti-inflammatory drugs such as ibuprofen and naproxen reduce inflammation by suppressing prostaglandins, chemicals that cause swelling and pain. When inflammation is reduced, the body's natural healing mechanisms can kick into action and promote a faster recovery.
Anesthetics, such as topical creams and patches, can also provide localized relief from pain and discomfort. The anesthetics used at home are much different than the ones used by emergency department anesthesiologists.
These over-the-counter medications work by numbing the application area, thus reducing pain signals that reach the brain. Anesthetic creams often have lidocaine as an active ingredient and can provide quick relief from pain and discomfort.
Physical Therapy
Physical therapy is a holistic approach to pain management that focuses on restoring movement, reducing pain, and improving function. Physical therapy aims to help individuals regain their independence, improve their quality of life, and reduce their dependence on pain medications.
Physical therapy can include exercises and stretches designed to strengthen the affected area, improve flexibility, and reduce pain.
Physical therapists also use manual therapy techniques, such as massage and joint mobilization, to reduce pain and improve mobility. In addition, physical therapists can provide education on posture and body mechanics, helping individuals prevent further injury and reduce their risk of chronic pain.
Physical therapy is the most recommended form of pain management for those suffering from chronic pain conditions, recovering from injuries, and managing musculoskeletal issues. While acute pain can sometimes resolve independently, physical therapy helps ensure that the body can recover correctly and function optimally.
Acupuncture
Complementary interventions offer a unique and holistic approach to managing pain when used to augment traditional techniques. These interventions aim to provide a well-rounded approach to alleviate discomfort and improve the overall quality of life.
Epidural
Epidural injections harness the power of modern science to provide immediate and effective pain relief. This minimally invasive procedure delivers medicine directly to the affected area.
It is often used to reduce pain in those suffering from chronic conditions, such as neck and back pain, as well as postoperative pain. With its safe and proven results, epidural injections offer a modern and efficient solution for pain management.
Why Should You Work With a Doctor?

Pain is a pervasive companion, often hidden yet all-consuming. Tackling its often complex and elusive nature is a task that requires a delicate balance of expertise and collaboration.
Like the interplay of instruments in a symphony, patients and healthcare providers must work harmoniously to create a solution to manage pain. Doctors, nurses, and physical therapists all bring their wealth of knowledge and experience to the stage.
Each type of practitioner can offer personalized recommendations and monitor the patient's progress. By carefully considering the patient's medical history, lifestyle, and treatment goals, medical professionals can create a comprehensive pain management plan to help their patients achieve physical comfort.
What Should You Know About Opioids?
Opioids may offer rapid and effective relief from pain — but they can also lead to dependence and addiction.
To truly maximize the benefits of these medications, it's essential to understand the intricate dance between their potency and their pitfalls. By approaching their use with caution and care, healthcare providers and patients alike can minimize the risks and maximize the rewards of this powerful form of pain management.
Guiding Principles for Opioid Use
In response to growing concerns over opioid use and its potential for abuse, government regulators have set forth guidelines for the use of opioids in the treatment of acute pain, particularly lower back pain.
Experts have provided comprehensive recommendations for responsible opioid prescription practices to ensure the safety and well-being of patients.
These guidelines highlight the critical importance of effective communication between clinicians and patients. They also highlight the importance of vigilant monitoring of a patient's progress, especially regarding pain intensity and the potential for side effects.
By following these guidelines, healthcare providers can ensure that their patients receive adequate pain relief while minimizing the associated risks of these potent medications.
A Provider's Responsibilities
For healthcare providers, the responsibility of managing opioid use cannot be taken lightly. To deliver safe and effective pain management, they must monitor their patient's use of these medications and be prepared to make adjustments as needed.
Whether it's adjusting the dose, switching to alternative medications, or using non-opioid options, providers play a crucial role in ensuring that patients receive the care they need while avoiding the dangers of overuse and abuse.
Why Is Pain Management So Crucial?
Pain is a universal experience that can affect all aspects of life. From chronic back pain that makes daily activities difficult to an injury that interrupts a young athlete's career, pain can rob us of our hobbies, passions, and work life.
Office workers who experience frequent headaches, for instance, may find it challenging to concentrate and be productive, leading to decreased job satisfaction and financial stress.
Effective pain management is crucial to tackling the various types of pain. From prescription pain medication to physical therapy and complementary interventions, several options are available to help individuals manage the intensity of their pain and regain control over their daily routines.
While prescription pain medication can provide short-term relief, it's essential to follow up with other forms of pain management to address the underlying issue and support the nervous system effectively. By addressing pain at its root, we can help reduce or eliminate debilitating symptoms and improve our overall quality of life.
The Bottom Line
Managing pain is a critical aspect of healthcare. Collaboration between patients and healthcare providers is essential in finding an effective pain management plan. This includes gauging the patient’s pain intensity, trigger points, medical history, and current health status and utilizing a multi-disciplinary approach that incorporates conventional and complementary therapies.
Regular follow-up appointments, monitoring of pain intensity, and adjustments to the pain management plan as needed are crucial in ensuring its success. By working with their providers, individuals can regain control over their pain and improve their overall well-being.
At Muscle MX, we aim to empower individuals with modern science to lead healthier, more active lives.
Sources:
Guideline at a Glance | CDC
Epidural: What It Is, Procedure, Risks & Side Effects | Cleveland Clinic
Physical therapy | NCBI Bookshelf