Did you know that calf muscle pain is a common complaint experienced by individuals across various age groups and activity levels? Whether you're an athlete, a weekend warrior, or someone who spends long hours on their feet, calf pain can disrupt daily activities and hinder mobility. Understanding the all-around nature of calf muscle pain is essential for effective management and prevention. That’s why we’ll be covering every aspect of calf muscle pain, offering valuable insights to help you recognize, treat, and prevent this condition.
What Is Calf Muscle Pain?
The calf is the muscle group located at the back of the lower leg, comprising two primary muscles: the gastrocnemius and the soleus. These muscles work together to facilitate movements such as walking, running, and jumping. Calf muscle pain refers to discomfort, soreness, or a sharp pain in this area. It can range from a mild ache to severe pain that impedes mobility.
Two Category Types of Calf Muscle Pain
Calf muscle pain is often categorized into two types:
-
Acute Calf Pain: Refers to sudden and severe pain in the calf muscles, as it typically results from a sudden injury, such as a muscle strain or tear. It can also occur due to cramping, tendonitis, blood clots, or compartment syndrome.
-
Chronic Calf Pain: Chronic calf pain is persistent discomfort or pain in the calf muscles that lasts for an extended period, typically more than a few weeks, due to causes such as muscle overuse, chronic tendonitis, poor circulation, nerve issues, muscle imbalance or weakness, previous injuries, or chronic conditions. Unlike acute calf pain, which comes on suddenly, this type of pain develops gradually and can be ongoing or recurrent.
Anatomy of the Calf Muscles
Before diving into the causes and symptoms of calf muscle pain, it's essential to understand the anatomy of the calf muscles. The calf comprises two primary muscles:
-
Gastrocnemius Muscle: The gastrocnemius is the larger of the two calf muscles and forms the bulk of the calf's shape. It has two heads, medial and lateral, which originate from the femur (thigh bone) and attach to the Achilles tendon. This muscle is responsible for plantar flexion (pointing the toes downward) and is highly active during activities like running and jumping.
-
Soleus Muscle: The soleus lies beneath the gastrocnemius and is a smaller, flatter muscle. It also contributes to plantar flexion but is more active during activities that require sustained, low-intensity contractions, such as standing and walking.
Together, these muscles impact various movements, making them susceptible to injury and strain.
What are the Different Kinds of Calf Muscle Pain Causes and Their Accompanied Symptoms and Treatments?
Calf muscle pain can be attributed to a variety of causes, ranging from minor strains to more serious medical conditions. So, identifying the underlying cause is essential for effective treatment.
Cause #1: Muscle Strain
Muscle strain, also known as a “pulled muscle”, is one of the most common causes of calf pain. It occurs when the muscle fibers are overstretched or torn, often due to sudden movements or excessive force. Muscle strains are common in athletes and individuals who engage in activities that require explosive movements, such as sprinting or jumping.
Symptoms of Muscle Strain:
- Sudden, sharp pain in the calf
- Swelling and bruising
- Difficulty walking or bearing weight on the affected leg
- Muscle weakness
Treatment for Muscle Strain:
-
Rest: Avoid activities that exacerbate the pain.
-
Ice: Apply ice to reduce swelling and pain.
-
Compression: Use an elastic bandage to provide support and reduce swelling.
-
Elevation: Keep the leg elevated to minimize swelling.
-
Physical Therapy: A structured rehabilitation program can help restore strength and flexibility.
Cause #2: Muscle Cramps
Muscle cramps are involuntary contractions of the calf muscles that can cause sudden and intense pain. They are often triggered by factors such as dehydration, electrolyte imbalances, or prolonged physical activity. Cramps can occur during exercise or at rest, and they are more common in older adults.
Symptoms of Muscle Cramps:
- Sudden, intense pain in the calf
- Muscle tightness or knotting
- Inability to relax the muscle
- Visible or palpable muscle contractions
Treatment for Muscle Cramps:
-
Stretching: Gently stretch the calf muscle to alleviate the cramp.
-
Hydration: Drink water or electrolyte-rich beverages to prevent dehydration.
-
Massage: Massaging the affected muscle can help relax the contraction.
-
Heat: Applying heat can soothe the muscle and prevent future cramps.
Cause #3: Achilles Tendonitis
Achilles tendonitis is inflammation of the Achilles tendon, which connects the calf muscles to the heel bone. This condition is often caused by overuse, particularly in athletes who engage in repetitive activities like running or jumping. It can also develop due to improper footwear or sudden increases in physical activity.
Symptoms of Achilles Tendonitis:
- Pain and stiffness along the Achilles tendon
- Swelling and tenderness near the heel
- Pain that worsens with activity
- Limited range of motion in the ankle
Treatment for Achilles Tendonitis:
-
Rest: Reduce or avoid activities that strain the Achilles tendon.
-
Ice: Apply ice to the affected area to reduce inflammation.
-
Physical Therapy: Exercises to strengthen the calf muscles and improve flexibility.
-
Orthotics: Custom shoe inserts can provide support and reduce strain on the tendon.
-
Anti-Inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation.
Cause #4: Deep Vein Thrombosis (DVT)
Deep vein thrombosis (DVT) is a serious condition where a blood clot forms in a deep vein, usually in the leg. While DVT is not primarily a muscle condition, it can cause calf pain and should be considered in the differential diagnosis. DVT is potentially life-threatening if the clot dislodges and travels to the lungs, causing a pulmonary embolism.
Symptoms of DVT:
- Persistent calf pain or tenderness
- Swelling in the affected leg
- Warmth and redness over the affected area
- Veins that are visibly swollen or discolored
Treatment for DVT:
-
Immediate Medical Attention: DVT requires prompt medical evaluation and treatment.
-
Anticoagulants: Blood-thinning medications are prescribed to prevent clot enlargement and reduce the risk of pulmonary embolism.
-
Compression Stockings: These can help reduce swelling and prevent clot formation.
-
Physical Activity: Light exercise can improve circulation and reduce the risk of further clotting.
Cause #5: Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD) occurs when the arteries that supply blood to the legs become narrowed or blocked due to atherosclerosis. This condition reduces blood flow to the muscles, leading to pain, especially during physical activity. PAD is more common in individuals with risk factors such as smoking, diabetes, and high cholesterol.
Symptoms of PAD:
- Calf pain that occurs during walking or exercise and subsides with rest (intermittent claudication)
- Coldness or numbness in the lower leg or foot
- Weak or absent pulse in the leg
- Slow-healing sores or wounds on the leg or foot
Treatment for PAD:
-
Lifestyle Changes: Quitting smoking, managing diabetes, and adopting a heart-healthy diet.
-
Medications: Cholesterol-lowering drugs, blood pressure medications, and antiplatelet agents.
-
Exercise: A supervised exercise program can improve circulation and reduce symptoms.
-
Surgical Intervention: In severe cases, procedures such as angioplasty or bypass surgery may be necessary to restore blood flow.
Cause #6: Compartment Syndrome
Compartment syndrome is a rare but serious condition that occurs when pressure within the muscles builds up to dangerous levels. This pressure can decrease blood flow, preventing oxygen and nutrients from reaching nerve and muscle cells. Compartment syndrome can be acute (following an injury) or chronic (due to repetitive activity).
Symptoms of Compartment Syndrome:
- Severe, persistent pain in the calf
- Swelling and tightness in the lower leg
- Numbness or tingling in the affected area
- Weakness or difficulty moving the foot
Treatment for Compartment Syndrome:
-
Immediate Medical Attention: Acute compartment syndrome is a medical emergency that requires prompt surgical intervention.
-
Fasciotomy: A surgical procedure to relieve pressure by cutting the fascia (the connective tissue surrounding the muscles).
-
Rest and Rehabilitation: For chronic compartment syndrome, reducing or modifying physical activity may help alleviate symptoms.
7. Calf Muscle Contusion
A calf muscle contusion, or bruise, occurs when the muscle is struck by a blunt force, causing blood vessels to rupture and bleed into the surrounding tissue. This can happen during sports, accidents, or falls.
Symptoms of Calf Muscle Contusion:
- Pain and tenderness at the site of the injury
- Swelling and bruising
- Difficulty walking or bearing weight
- Stiffness and reduced range of motion
Treatment for Calf Muscle Contusion:
-
Rest: Avoid activities that worsen the pain.
-
Ice: Apply ice to reduce swelling and pain.
-
Compression: Use a bandage to provide support and minimize swelling.
-
Elevation: Keep your leg elevated to reduce swelling.
-
Pain Relief: Over-the-counter pain medications can help manage discomfort.
A Summary of Symptoms of Calf Muscle Pain
Calf muscle pain can present with various symptoms depending on the underlying cause. While the primary symptom is pain in the calf area, the nature and severity of the pain can vary. Below are some common symptoms associated with calf muscle pain:
-
Sharp or Stabbing Pain: This type of pain is often indicative of a muscle strain or tear. It may occur suddenly during physical activity and can be severe enough to halt movement.
-
Dull Ache: A persistent, dull ache in the calf may be a sign of overuse or a chronic condition like Achilles tendonitis or PAD. The pain may worsen with activity and improve with rest.
-
Swelling: Swelling in the calf can occur with injuries such as muscle strains, contusions, or DVT. The swelling may be localized to the injured area or affect the entire lower leg.
-
Bruising: Bruising, or discoloration of the skin, often accompanies a muscle contusion or severe strain. The bruise may appear immediately after the injury or develop over time.
-
Muscle Weakness: Muscle weakness in the calf can result from a strain, tear, or nerve involvement. Weakness may make it difficult to walk, stand, or perform activities that require calf strength.
-
Tightness or Stiffness: Tightness or stiffness in the calf muscles is common after prolonged physical activity or with conditions like muscle cramps and compartment syndrome. The muscle may feel tight to the touch and resist stretching.
-
Numbness or Tingling: Numbness or tingling in the calf or foot may indicate nerve involvement, as seen in conditions like compartment syndrome or nerve compression. These symptoms should be evaluated by a healthcare provider.
-
Limited Range of Motion: Injuries or conditions affecting the calf muscles may result in limited range of motion in the ankle and foot. This can make it challenging to perform everyday activities.
-
Warmth or Redness: Warmth and redness over the calf area may indicate inflammation, infection, or a condition like DVT. These symptoms warrant immediate medical attention.
Diagnosis of Calf Muscle Pain
Diagnosing the underlying cause of calf muscle pain is crucial for determining the appropriate treatment plan. A thorough evaluation by a healthcare professional typically involves the following steps:
Step #1: Reviewing Your Medical History
The healthcare provider will begin by taking a detailed medical history, including information about the onset, duration, and nature of the pain. They may ask about recent physical activity, previous injuries, and any underlying medical conditions. Understanding your medical history helps narrow down potential causes.
Step #2: Physical Examination
A physical examination of the calf and surrounding areas will be performed to assess the extent of the pain, swelling, and any visible signs of injury. The healthcare provider may check for tenderness, muscle strength, range of motion, and any abnormalities in the skin or blood vessels.
Step #3: Imaging Studies
Imaging studies such as X-rays, ultrasound, or MRI may be ordered to evaluate the muscles, tendons, and bones in the calf. These tests can help identify muscle tears, fractures, blood clots, or other underlying conditions that may be causing the pain.
X-Rays
X-rays are primarily used to visualize bones and detect fractures or other bone-related issues. While they are not directly useful for diagnosing soft tissue injuries like muscle strains, X-rays can rule out bone fractures or abnormalities that might contribute to calf pain. X-rays pass through the body, with denser materials like bones absorbing more radiation and appearing white on the image, while softer tissues appear darker. X-rays do not show soft tissues like muscles, tendons, or ligaments clearly, so they are not typically used for diagnosing muscle injuries but can be part of an initial assessment.
Ultrasound
Ultrasound is particularly useful for assessing soft tissue injuries, such as muscle tears, strains, and tendon damage. It can also help in detecting fluid collections, like hematomas, within the calf muscle. Ultrasound uses high-frequency sound waves to create real-time images of the soft tissues. The waves reflect differently off various tissues, allowing the creation of an image that shows muscle structure, tears, and other abnormalities. Ultrasound is non-invasive, does not use radiation, and can provide dynamic images, meaning it can show the muscle in motion, which is useful for assessing muscle function. Keep in mind that the quality of the ultrasound image can be operator-dependent, and it may not provide as much detail as an MRI.
MRIs (Magnetic Resonance Imaging)
MRI is the most detailed imaging technique for assessing soft tissue injuries, including calf muscle injuries. It provides a comprehensive view of muscles, tendons, ligaments, and surrounding tissues, making it ideal for diagnosing the extent of muscle tears, strains, or other soft tissue injuries. MRI uses a strong magnetic field and radio waves to create detailed cross-sectional images of the body. It can differentiate between different types of tissues based on their water content, making it highly effective for soft tissue evaluation. MRI provides high-resolution images and is very sensitive in detecting even small injuries. It’s the gold standard for diagnosing complex soft tissue injuries. However, MRI is also more expensive than other imaging methods and typically takes longer to perform. It also may not be suitable for patients with certain types of metal implants or devices.
Step #4: Blood Tests
In some cases, blood tests may be ordered to check for underlying conditions such as infections, electrolyte imbalances, or blood clotting disorders. Blood tests can help identify systemic issues that may contribute to calf pain.
Step #5: Specialized Tests
If peripheral artery disease (PAD) is suspected, specialized tests such as the ankle-brachial index (ABI) may be performed to assess blood flow to the legs. In cases of suspected compartment syndrome, a compartment pressure test may be conducted to measure the pressure within the muscle compartments.
Primary Treatments of Calf Muscle Pain
The treatment of calf muscle pain depends on the underlying cause and the severity of the condition. While mild cases may resolve with self-care and conservative measures, more severe injuries or conditions may require medical intervention. Here are the primary treatment options for calf muscle pain:
Primary Treatment #1: Rest and Activity Modification
Rest is a fundamental component of treating calf muscle pain, especially in cases of muscle strain, tendonitis, or contusion. Avoiding activities that exacerbate the pain allows the muscles and tissues to heal. Gradual return to activity is recommended to prevent re-injury.
If complete rest is not possible though, modifying activities to reduce stress on the calf muscles can be beneficial. For example, switching from high-impact activities like running to low-impact exercises like swimming or cycling can help maintain fitness while allowing the calf to recover.
Primary Treatment #2: Ice and Heat Therapy
Ice and heat therapy are commonly used to manage calf muscle pain and inflammation. To better break these down for a moment:
-
Ice Therapy: Applying ice to the affected area for 15-20 minutes several times a day can help reduce swelling and numb the pain. Ice is most effective in the first 48 hours after an injury.
-
Heat Therapy: Heat therapy, such as warm compresses or heating pads, can help relax tight muscles and improve blood flow. Heat is typically recommended after the initial swelling has subsided.
Primary Treatment #3: Compression and Elevation
Compression and elevation are effective methods for reducing swelling and promoting healing in cases of calf muscle pain:
-
Compression: Using an elastic bandage or compression sleeve can help reduce swelling by applying gentle pressure to the calf. Be careful not to wrap too tightly, as this can impede circulation.
-
Elevation: Elevating the leg above heart level can help reduce swelling by encouraging fluid drainage from the affected area. This is particularly useful in cases of muscle contusion or DVT.
Primary Treatment #4: Medications
Over-the-counter and prescription medications can be used to manage pain and inflammation associated with calf muscle pain:
-
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs such as ibuprofen or naproxen are commonly used to reduce pain and inflammation. These medications are effective for managing symptoms of muscle strain, tendonitis, and other inflammatory conditions.
-
Pain Relievers: Acetaminophen (Tylenol) can be used to manage pain if NSAIDs are contraindicated.
-
Prescription Medications: In some cases, stronger pain relievers or muscle relaxants may be prescribed by a healthcare provider.
Primary Treatment #5: Physical Therapy
Physical therapy plays a crucial role in the rehabilitation and recovery of calf muscle pain. A physical therapist can design a personalized exercise program to improve strength, flexibility, and range of motion in the calf muscles, such as:
-
Stretching Exercises: Stretching exercises help improve flexibility and prevent muscle tightness. Calf stretches, such as the wall stretch or towel stretch, can be performed daily to maintain muscle length.
-
Strengthening Exercises: Strengthening exercises, such as calf raises and resistance band exercises, can help rebuild muscle strength and prevent future injuries.
-
Manual Therapy: Techniques such as massage, myofascial release, and joint mobilization can help relieve muscle tension and improve circulation.
Primary Treatment #6: Orthotics and Footwear
Proper footwear and orthotic devices can provide support and alleviate stress on the calf muscles, especially in cases of Achilles tendonitis or plantar fasciitis. Let’s break down these two types for a second here:
-
Orthotics: Custom orthotic inserts can help correct foot biomechanics and reduce strain on the calf muscles. They are particularly beneficial for individuals with flat feet or high arches.
-
Supportive Footwear: Wearing shoes with good arch support, cushioning, and shock absorption can prevent calf muscle pain and reduce the risk of injury.
Primary Treatment #7: Surgical Intervention
In severe cases, surgical intervention may be necessary to address the underlying cause of calf muscle pain. Surgery is typically considered when conservative treatments have failed or when there is a risk of long-term complications. The three most common types are:
-
Fasciotomy: In cases of acute compartment syndrome, a fasciotomy may be performed to relieve pressure within the muscle compartments and restore blood flow.
-
Tendon Repair: Surgical repair of a torn Achilles tendon may be required for individuals with a complete rupture.
-
Vascular Surgery: In cases of severe peripheral artery disease, vascular surgery such as angioplasty or bypass surgery may be performed to restore blood flow to the legs.
Primary Treatment #8: Lifestyle Modifications and Prevention
Preventing calf muscle pain requires adopting healthy lifestyle habits and taking proactive measures to reduce the risk of injury. Here are some tips for preventing calf muscle pain:
-
Stay Hydrated: Proper hydration is essential for muscle function and can help prevent muscle cramps. Drink water regularly, especially during physical activity.
-
Warm-Up and Stretch: Always warm up before engaging in physical activity and perform dynamic stretches to prepare the muscles for movement. After exercise, incorporate static stretching to maintain flexibility.
-
Gradual Progression: Avoid sudden increases in the intensity or duration of physical activity. Gradually build up your exercise routine to allow the muscles to adapt.
-
Maintain a Healthy Weight: Excess weight can place additional stress on the calf muscles and increase the risk of injury. Maintaining a healthy weight through diet and exercise can reduce this risk.
-
Listen to Your Body: Pay attention to early signs of calf muscle pain or discomfort and address them promptly. Rest and modify activities as needed to prevent further injury.
Using CBD as an Option for Calf Muscle Pain
Cannabidiol (CBD) has gained attention as a potential aid for those seeking a natural option to ease muscle discomfort, including in the calves. CBD is a compound derived from the cannabis plant, but unlike THC, it does not have psychoactive properties. Instead, CBD interacts with the body’s endocannabinoid system (ECS), which has a role in regulating various physiological processes, including the response to physical stress and the sensation of discomfort.
So, when it comes to addressing calf muscle discomfort, CBD, based on both research and anecdotal evidence, may be able to provide the following:
-
Support for Muscle Tension: After a workout or a long day on your feet, your calf muscles might feel tight and stiff. CBD is believed to support the body’s natural ability to manage muscle tension, potentially helping your calves feel more relaxed.
-
Enhancing Relaxation: CBD is known for its blissful properties. Applying CBD topically or taking it orally may promote a sense of overall relaxation, which could be beneficial for muscles that feel tense or overworked.
-
Potential for Reducing Swelling: Physical activity can sometimes lead to mild swelling in the muscles. CBD might support the body's natural mechanisms for managing swelling, making it a viable option to consider when your calves feel swollen or heavy.
-
Post-Exercise Recovery: Athletes often look for ways to optimize their recovery after intense workouts. CBD could be a useful addition to your post-exercise routine, supporting the body’s natural recovery processes and helping you get back on your feet more comfortably.
-
Improving Sleep Quality: Quality sleep is essential for muscle recovery. CBD has been reported to help some individuals achieve better sleep, which in turn can aid in the recovery of tired or strained muscles, including those in the calves.
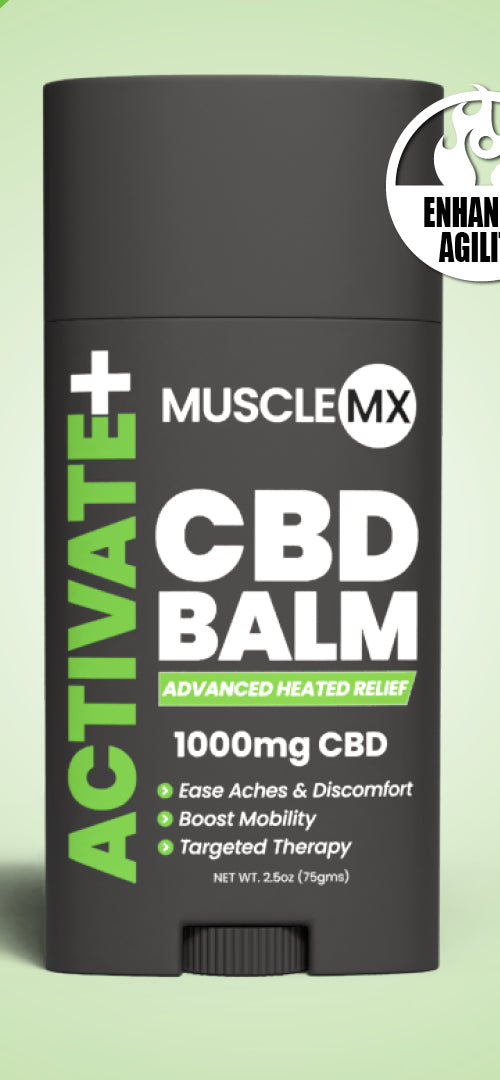
Now, in term of CBD product types/delivery methods, topical solutions, such as balms, lotions, and creams are the top option here. You see, these topicals are infused with cannabidiol, which can be applied directly for targeted comfort, i.e. to the calf muscles. This in turn allows the CBD to be absorbed through the skin, targeting the specific area of discomfort. You could also try, especially after a long day, a warm bath infused with CBD. This can help soothe tired muscles. CBD bath salts or bombs can provide a relaxing experience, allowing your calf muscles to unwind in the process.
Don’t Let Calf Muscle Pain Get in Your Way of Moving Around!
Calf muscle pain is a common condition with a wide range of causes, from minor muscle strains to serious medical conditions like deep vein thrombosis or peripheral artery disease. So, understanding the underlying cause of calf muscle pain is crucial for effective treatment and prevention.
Again, CBD presents a natural option that may help manage calf muscle discomfort without the use of synthetic products. Whether you’re an athlete recovering from a strenuous workout or someone who’s spent a long day on their feet, incorporating cannabidiol into your wellness routine could offer the support you need for your calf muscles. Remember to consult with your doctor/physician before starting any new supplement – and once given the okay to do so, go with Muscle MX CBD Topical products, as we made sure they meet the highest standards of quality and effectiveness possible.