Can Physical Therapy Help Arthritis?
Arthritis is a condition that millions of people face daily, and its impact can range from mild discomfort to debilitating pain. While there’s no magical solution to cure arthritis completely, there are methods that can significantly improve quality of life, reduce symptoms, and restore mobility. Physical therapy has emerged as a beacon of hope for those living with arthritis, offering a structured approach to manage symptoms and regain control over their lives.
What is Arthritis?
Arthritis is not a single condition but an umbrella term for various disorders that affect the joints. At its core, arthritis involves inflammation or degeneration of the joints, leading to pain, stiffness, and reduced mobility. The condition can affect anyone, regardless of age, although it is more prevalent among older adults.
The most common symptoms include:
- Joint pain and stiffness.
- Swelling and redness around the affected area.
- Decreased range of motion.
- A sensation of warmth in the joints.
Arthritis isn’t just a physical condition; it can also take a toll on mental health, contributing to stress and reduced quality of life. Understanding the type of arthritis you’re dealing with is critical to determining the best course of action, including whether physical therapy might be beneficial.
What are the Different Kinds/Types of Arthritis?
There are over 100 types of arthritis, each with unique causes, symptoms, and treatment strategies. Here are the most common ones:
-
Osteoarthritis (OA): Known as "wear-and-tear" arthritis, OA occurs when the cartilage cushioning the ends of bones wears down over time. Symptoms include joint pain, stiffness, and loss of flexibility, often in the knees, hips, hands, or spine. Aging, joint overuse, injury, or obesity are typically causes of this.
-
Rheumatoid Arthritis (RA): An autoimmune disorder where the immune system attacks the joint lining, causing inflammation and damage. Symptoms include swollen, warm, and painful joints; fatigue; and symmetrical joint involvement (e.g., both hands or knees). Exact cause is unknown, but it involves genetic and environmental factors.
-
Psoriatic Arthritis (PsA): Often occurs in people with psoriasis, a skin condition, and affects both skin and joints. Symptoms include joint pain, stiffness, and swelling, often accompanied by skin plaques. Immune system malfunction, genetic predisposition, or environmental triggers are the main causes.
-
Gout: A form of arthritis caused by the accumulation of uric acid crystals in the joints. Symptoms include intense pain, swelling, and redness, often affecting the big toe but can occur in other joints. Causes stem from high levels of uric acid due to diet, alcohol consumption, or certain health conditions.
-
Ankylosing Spondylitis (AS): A type of inflammatory arthritis primarily affecting the spine and sacroiliac joints. Symptoms include chronic back pain, stiffness, and in severe cases, fusion of the spinal bones. Genetic factors are the cause here, particularly the HLA-B27 gene.
-
Juvenile Idiopathic Arthritis (JIA): The most common form of arthritis in children, characterized by inflammation in one or more joints. Symptoms such as swelling, stiffness, and pain in joints, sometimes accompanied by fever or rash occur. The causes are unknown, but it may involve genetic and immune factors.
-
Lupus (Systemic Lupus Erythematosus - SLE): A systemic autoimmune disease that can cause inflammation in joints, skin, kidneys, and other organs. Joint pain, fatigue, butterfly-shaped facial rash, and other systemic symptoms. In terms of causes, there is immune dysfunction, potentially triggered by environmental or hormonal factors.
-
Fibromyalgia: Though not technically a form of arthritis, it is often grouped with arthritis conditions due to widespread musculoskeletal pain. Chronic pain, fatigue, and tender points across the body are typically the symptoms. Causes are unknown, though it may involve nervous system dysfunction.
-
Reactive Arthritis: Inflammation of the joints triggered by an infection elsewhere in the body. Symptoms include joint pain and swelling, often in knees, ankles, and feet, along with inflammation of the eyes or urinary tract. Bacterial infections, such as those causing food poisoning or sexually transmitted infections are the usual causes.
-
Infectious Arthritis (Septic Arthritis): Arthritis caused by a bacterial, viral, or fungal infection in a joint. Severe joint pain, swelling, redness, and fever are the accompanied symptoms here. Infections like staph or gonorrhea entering the joint can be the causes here.
-
Undifferentiated Arthritis: Arthritis that does not fit the specific criteria for any type of arthritis. Symptoms are similar to other arthritis types, including joint pain and inflammation. Often a precursor to a more defined arthritis type.
-
Polymyalgia Rheumatica: An inflammatory disorder causing muscle pain and stiffness, particularly in the shoulders and hips. Severe pain and stiffness, especially in the morning or after rest are symptoms that can happen. Exact cause is unknown though, but it may involve immune or genetic factors.
-
Enteropathic Arthritis: Associated with inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis. Joint pain and stiffness, often in conjunction with gastrointestinal symptoms. The direct cause is immune system dysregulation linked to IBD.
-
Seronegative Arthritis: A group of arthritic diseases where tests for rheumatoid factor are negative, including PsA, AS, and reactive arthritis. Symptoms vary by condition, but often include joint pain and inflammation. Typically caused by immune or genetic factors.
- Crystal Arthropathies (Other than Gout): Pseudogout (calcium pyrophosphate deposition disease - CPPD). Symptoms are similar to gout, with sudden joint pain and swelling. The direct cause is deposition of calcium crystals in the joint.
Each type of arthritis has its nuances, but physical therapy can often help manage symptoms regardless of the specific diagnosis.
How Long Does Arthritis Typically Last For and Can It Progress?
Arthritis is generally a long-term condition, though its duration and progression vary depending on the type and individual factors such as age, lifestyle, and overall health. Some forms, like gout, manifest in sudden flare-ups that subside after treatment, while others, like osteoarthritis and rheumatoid arthritis, are chronic and require ongoing management.
Does Arthritis Progress Over Time?
Yes, arthritis can progress, especially if left unmanaged. For instance:
-
Osteoarthritis gradually worsens as cartilage continues to degrade.
-
Rheumatoid Arthritis can cause permanent joint deformities if untreated.
-
Psoriatic Arthritis may lead to severe joint and bone damage over time.
Timely intervention, including physical therapy, lifestyle changes, and medical treatments, can significantly slow down the progression and improve functionality.
What Does a Physical Therapist Do for Arthritis?
Physical therapists (PTs) play a vital role in managing arthritis by focusing on restoring mobility, reducing pain, and improving overall joint health. Here’s how they can help:
-
Personalized Exercise Plans: PTs create exercise regimens tailored to your specific needs, ensuring the movements are safe and effective for your joints. These exercises often aim to strengthen the muscles around the joints, reducing the load and improving stability.
-
Pain Management Techniques: From manual therapy to heat and cold applications, PTs use a variety of techniques to alleviate discomfort.
-
Education on Joint Protection: Learning how to move and carry out daily activities without exacerbating joint stress is an essential part of physical therapy.
-
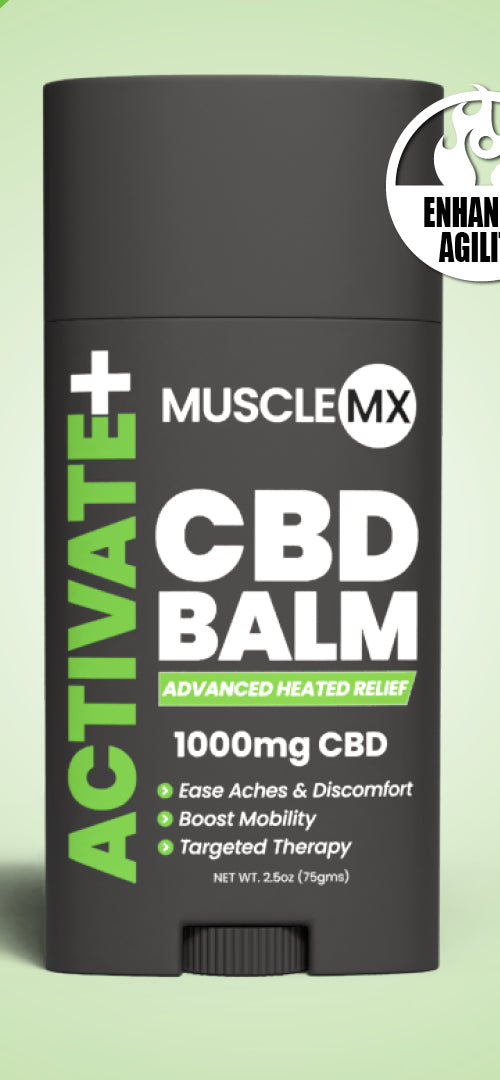
Stretching and Flexibility Training: Gentle stretches improve range of motion and reduce stiffness, making daily tasks more manageable. For instance, if you’re dealing with hip pain, combining stretching with complementary methods like CBD balms and CBD lotions could subtly amplify relaxation without overloading your regimen.
-
Assistive Devices and Modifications: PTs can recommend braces, orthotics, or ergonomic tools to make life easier and safer for arthritis patients.
-
Post-Surgery Rehabilitation (if applicable): After joint replacement or other arthritis-related surgeries, a PT helps with recovery by improving strength, mobility, and overall function.
How Long Does Physical Therapy for Arthritis Last?
The duration of physical therapy for arthritis varies depending on the severity of the condition, the type of arthritis, and the individual's response to treatment. However, a typical course of physical therapy may last anywhere from 6 weeks to 3 months. In fact, there are certain factors affecting duration:
-
Severity of Arthritis: If the arthritis is mild, therapy may last for a shorter period, while more severe cases could require ongoing therapy.
-
Type of Arthritis: For example, osteoarthritis may require less intensive therapy compared to rheumatoid arthritis, which is a more aggressive inflammatory condition.
-
Treatment Goals: If the goal is to reduce pain and improve mobility, therapy may be shorter. However, if the focus is on improving strength, function, or long-term management, it may take longer.
-
Individual Progress: Some people respond quickly to therapy, while others may need longer sessions to see improvements.
-
Physical Therapist's Recommendations: The frequency and duration of therapy can also depend on the physical therapist's assessment and the specific treatment plan tailored to the individual.
Generally, physical therapy sessions are scheduled 1-2 times per week, but the therapist may adjust this depending on progress. After the initial treatment phase, some patients may transition to a maintenance program, which might involve fewer sessions or at-home exercises.
What is the Best Exercise for Arthritis?
There’s no one-size-fits-all exercise for arthritis, but certain activities are universally beneficial:
-
Low-Impact Aerobic Exercises: Activities like walking, swimming, and cycling improve cardiovascular health without putting undue stress on the joints.
-
Strength Training: Building muscle around affected joints helps offload stress and improve stability. Exercises using resistance bands or light weights are excellent choices.
-
Range of Motion Exercises: These exercises, such as gentle stretches, keep joints flexible and reduce stiffness.
-
Water Therapy: Exercising in a pool offers resistance while minimizing joint impact, making it ideal for arthritis sufferers.
-
Yoga and Tai Chi: These practices combine stretching, strength, and mindfulness, providing both physical and mental benefits.
Always consult with your physical therapist to identify the exercises best suited to your needs.
Does Physical Therapy Get Rid of Inflammation?
It’s important to clarify that physical therapy doesn’t directly eliminate inflammation, especially in conditions like rheumatoid arthritis, where systemic inflammation is driven by the immune system. However, physical therapy can indirectly reduce inflammation’s impact by improving joint function and reducing mechanical stress. Specifically, here’s how physical therapy helps with inflammation:
-
Promoting Circulation: Gentle exercises increase blood flow, which can help reduce localized swelling and stiffness.
-
Improving Lymphatic Drainage: Movement encourages lymphatic flow, aiding in the reduction of swelling.
-
Strengthening Supporting Muscles: By offloading stress from the joints, inflammation-triggering factors like repetitive strain are minimized.
Physical therapy works best in conjunction with other treatments, such as medication or lifestyle adjustments. While it doesn’t "cure" inflammation, it creates an environment where the body can manage it more effectively.
Final Physical Therapy for Arthritis Thoughts
Living with arthritis can feel like an uphill battle, but physical therapy offers a proactive path toward relief and improved mobility. While it doesn’t promise a miracle cure, it empowers individuals with tools and strategies to reclaim control over their lives. Whether you’re dealing with mild stiffness or more severe joint challenges, a personalized therapy plan can make all the difference.
Physical therapy is more than just exercises—it’s a journey of understanding your body, finding your limits, and discovering how to live within or surpass them. So, take that first step. With guidance from a skilled physical therapist, arthritis doesn’t have to define your life; it can simply be a part of your story.