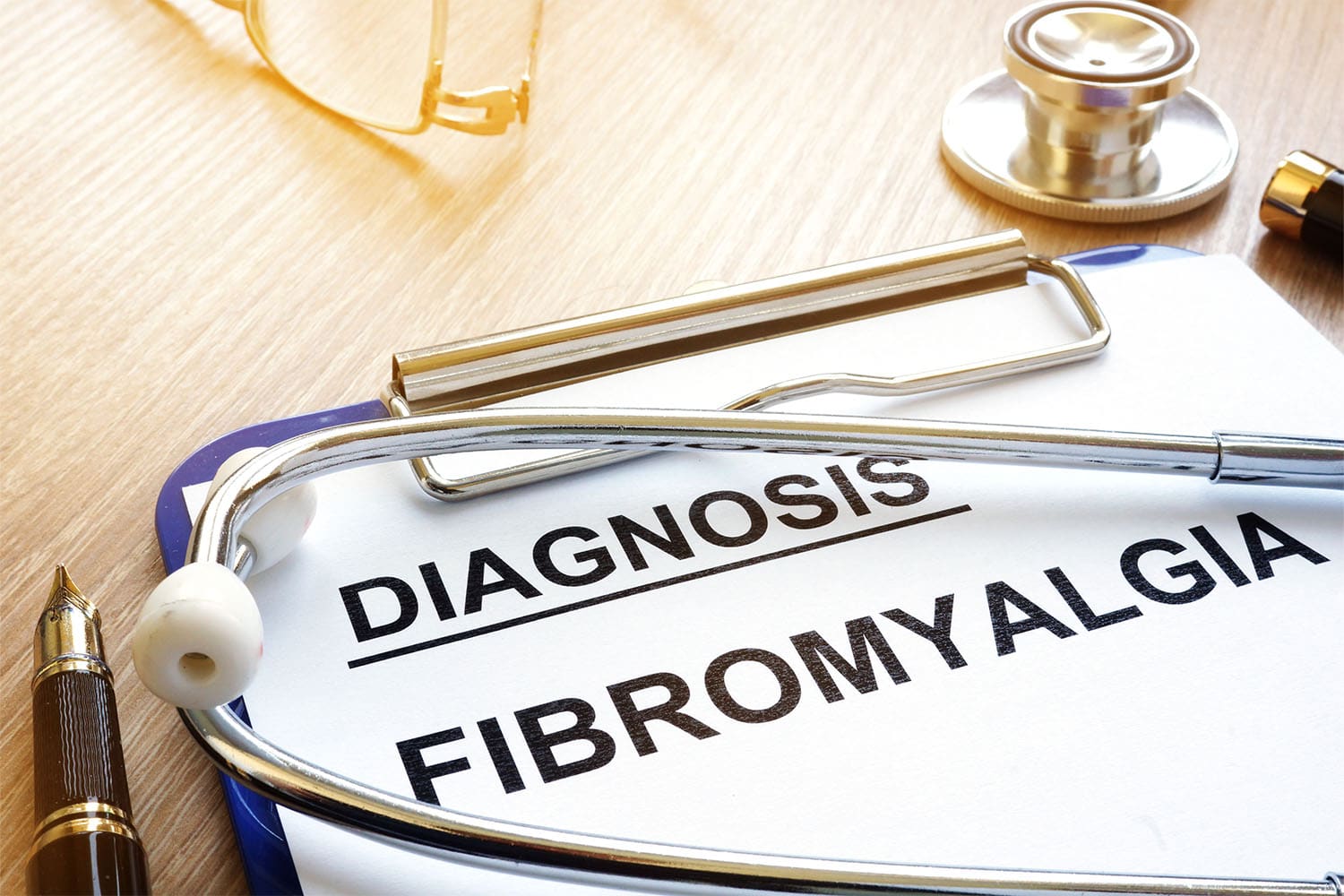
Is Fibromyalgia an Autoimmune Disease?
|
| Fibromyalgia syndrome (FMS) is a silent tormentor, affecting millions of people worldwide with widespread pain and tenderness that can be debilitating. This chronic pain condition is estimated to impact two to four percent of the world's population, yet its exact cause remains a mystery. |
Living with constant pain and tenderness can be overwhelming for those with fibromyalgia. Furthermore, many people are unaware of the condition, so it can be difficult for those living with fibromyalgia to get a proper diagnosis and access effective treatment.
In this blog, we aim to shed light on the ongoing debate about the potential autoimmune nature of fibromyalgia and the current state of treatments and therapies. In addition, we hope to bring hope and understanding to those affected by this debilitating condition by exploring the latest research and advancements.
What Are the Symptoms of Fibromyalgia?

For those that fibromyalgia affects, every day is a battle against widespread pain and tenderness in their muscles, tendons, and ligaments. This chronic pain condition can affect everyday functions like grip strength and also bring on a host of other unpleasant symptoms.
These can include:
-
Chronic fatigue syndrome: Feeling tired even after a good night's sleep.
-
Sleep disturbances: Difficulty falling or staying asleep.
-
Cognitive difficulties: Trouble concentrating and trouble with short-term memory, sometimes referred to as “fibro fog.”
-
Irritable bowel syndrome: A condition of the gastrointestinal tract that causes abdominal discomfort and changes in bowel movements.
-
Tender points: Areas of tenderness or pain often found around the neck, shoulder blades, elbows, and hips.
What Is an Autoimmune Disorder?
Think of the immune system as a well-trained army ready to defend the body against any foreign invaders that may cause harm. However, with autoimmune disorders, the immune system can sometimes mistakenly attack the body's own cells and tissues.
This misguided attack leads to chronic inflammation and tissue damage. The result is a body in a constant state of battle, causing widespread pain and discomfort.
What Makes a Condition an Autoimmune Disorder?
Diagnosing an autoimmune disorder involves a multidisciplinary approach that integrates clinical criteria and laboratory testing. Clinical criteria, including a comprehensive assessment of the patient's medical history and physical examination, serve as the cornerstone of the diagnostic process.
The medical history evaluation entails a detailed inquiry into the patient's symptoms, including their onset, duration, and exacerbating factors. The physical examination focuses on identifying signs and symptoms that may indicate an autoimmune disorder, such as joint pain, skin rashes, and fatigue.
Laboratory testing also plays a crucial role in the diagnostic process, providing objective evidence of autoimmune disorders. Blood tests, for example, can be utilized to determine the levels of specific immune molecules, such as autoantibodies, which are associated with autoimmune disorders.
In addition, other laboratory tests, such as imaging studies, can be performed to visualize tissue damage and inflammation, providing further evidence of autoimmune pathology.
Is Fibromyalgia an Autoimmune Disorder?
There's conflicting evidence as to whether fibromyalgia is an autoimmune disorder or not. On the one hand, some studies have found biochemical abnormalities and autoantibodies in patients with the condition. But, on the other hand, it's hard to find definitive proof that the body's immune system is attacking its own cells and tissues.
Evidence for Fibromyalgia as an Autoimmune Disease
The presence of autoantibodies in fibromyalgia patients has been observed in multiple studies. Elevated autoantibodies, such as anti-nuclear antibodies (ANA) and anti-dsDNA antibodies, have been found in individuals with fibromyalgia.
These autoantibodies are typically associated with autoimmune disorders, suggesting that fibromyalgia may have an autoimmune component.
Additionally, there is a strong association between fibromyalgia and other autoimmune disorders, such as rheumatoid arthritis and Sjögren's syndrome. In these disorders, the immune system is known to attack its own cells and tissues, and the same may be true for fibromyalgia.
This association suggests that there may be common underlying mechanisms involved in the development of these conditions and that fibromyalgia may be a manifestation of an underlying autoimmune process.
Evidence Against Fibromyalgia as an Autoimmune Disease
Despite the evidence supporting fibromyalgia as an autoimmune disorder, there are arguments against this theory. One argument is the lack of consistent antibody levels in fibromyalgia patients.
While some studies have found elevated levels of autoantibodies, others have not. This inconsistent finding makes it difficult to determine the role of autoimmunity in the development of fibromyalgia.
In autoimmune disorders, the immune system launches an attack against the body's own cells and tissues, leading to inflammation and tissue damage. However, studies of individuals with fibromyalgia have not consistently found evidence of immune cell infiltration in affected tissues, suggesting that an autoimmune mechanism may not be involved.
When taken together, the evidence for and against fibromyalgia as an autoimmune disorder is conflicting. While evidence suggests that an autoimmune mechanism may be involved, it’s currently inconclusive.
Drawing Conclusions
While we're not ready to make a definitive statement, the recent research coming out in the past few years may support the idea that fibromyalgia might be an autoimmune disorder. One study suggested that reducing the level of antibodies in the blood of fibromyalgia patients may help to relieve their symptoms.
Studies like these are helping to shed light on the mysterious nature of fibromyalgia; however, more research is needed to understand the role of autoimmunity in this condition entirely. As scientists continue to explore the role of immunological mechanisms, we may soon have a better understanding of what causes fibromyalgia and how to treat it.
But for now, we know that fibromyalgia is correlated with autoimmune-like mechanisms, which may be an important clue in developing new treatments and finding relief for patients.
How Is Fibromyalgia Treated?

Living with fibromyalgia pain can be overwhelming. While some patients only experience partial remission, most will require ongoing maintenance to reduce symptoms and improve their quality of life. This is why healthcare professionals must provide ongoing support and guidance to help patients become experts in self-managing their condition.
Cognitive Therapies
Despite these difficulties, there is growing evidence that self-management skills training is most effective when delivered in a small, supportive group setting.
Cognitive therapy, in particular, can be an effective treatment for fibromyalgia by helping patients recognize and challenge their negative thoughts about the condition. During cognitive therapy, patients can also learn how to reduce their stress levels and develop coping strategies for dealing with pain, fatigue, and other symptoms.
Regular Physical Activity
Exercise and psychoeducational approaches are effective ways to manage pain from fibromyalgia, but these therapies must be tailored to each patient. For example, to promote daily physical activity, patients may find it helpful to use a fitness wearable to track and record movement, along with a personalized treatment program.
Pharmacological Interventions
Pharmacological approaches can also help manage symptoms, but it's important to note that not all patients will tolerate or benefit from these drugs. Therefore, all drugs should be started at low doses and increased gradually, and providers should recommend drugs that target the predominant symptoms, such as pain, sleep disturbance, and psychological distress.
If a drug is not helping, patients should stop taking it based on the medical advice of their primary healthcare provider.
Antidepressants, such as low-dose amitriptyline, have traditionally been used to treat pain and sleep disturbance in fibromyalgia. Duloxetine and milnacipran have also been approved for the treatment of fibromyalgia, but they require a private prescription.
Antiepileptic drugs, such as pregabalin and gabapentin, may potentially manage pain and improve sleep, but weight gain can limit their effectiveness. On the other hand, opioids, such as codeine, fentanyl, and oxycodone, are not recommended due to poor clinical response and increased risk of opioid-induced dependence.
For those struggling with fibromyalgia, it's crucial to remember that you are not alone in this battle. Despite the difficulties, there are many resources and treatments available that can help you manage your symptoms and live a more fulfilling life.
What Is the Future of Fibromyalgia Research?
Imagine a world where fibromyalgia is no longer a mystery — a world where we understand the underlying causes and have effective treatments to help those who have this debilitating condition. This is the goal of ongoing and future research in fibromyalgia.
Ongoing Studies
Currently, rheumatology experts are looking into the role of the central nervous system in fibromyalgia and exploring the potential ability to transfer fibromyalgia symptoms. These studies hold great promise, and we can only hope they bring us one step closer to finding the answers we seek.
Potential Future Therapies
The future of fibromyalgia treatment looks bright. Soon, new medicines may target specific receptors in the musculoskeletal and nervous systems, and new blood tests may identify fibromyalgia and potential risk factors.
With some optimism and rapid advancement in medical technology, we can hopefully look forward to a day when fibromyalgia is better understood and more effectively managed, allowing those dealing with it to lead more fulfilling lives.
The Bottom Line
Living with fibromyalgia is like navigating a stormy sea – unpredictable and full of uncertainty. However, with the right resources and support, individuals can learn to manage their symptoms and live a more fulfilling life.
There are a variety of treatments available, including lifestyle changes and pharmacological interventions, as well as ongoing research that holds the promise of new and better treatments in the future.
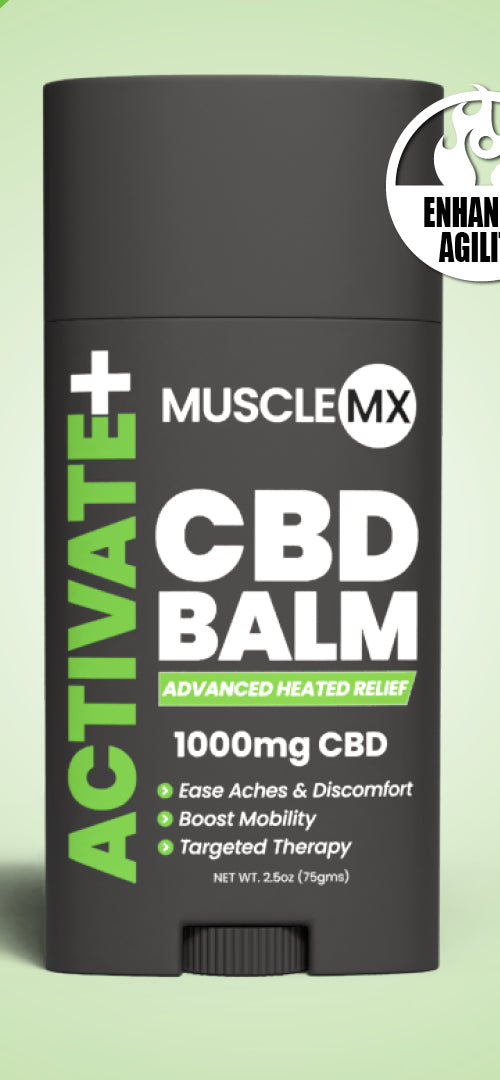
While medical treatments can effectively manage symptoms, doing things to help support your well-being are also crucial. At Muscle MX, we strive to lead the charge in developing innovative, holistic solutions that do just that. Muscle MX is empowering people to take control of their health and live the life they deserve.
Sources:
Fibromyalgia likely the result of autoimmune problems | ScienceDaily
Fibromyalgia: Neurological or autoimmune? | Practical Patient Care
Passive transfer of fibromyalgia symptoms from patients to mice | National Library of Medicine
JCI - Passive transfer of fibromyalgia symptoms from patients to mice| Journal of Clinical Investigation