Is It Situational Depression? Hidden Signs You Shouldn't Ignore
Key Takeaways
Understanding situational depression and recognizing its warning signs can prevent it from escalating into more serious mental health conditions.
-
Situational depression affects 10% of adults and differs from clinical depression by being triggered by specific stressful events rather than biological factors.
-
Watch for hidden warning signs: persistent fatigue, loss of interest in enjoyable activities, unexplained irritability, and social withdrawal that lasts beyond normal grief.
-
Seek professional help immediately if symptoms persist beyond 6 months, disrupt daily functioning, or include thoughts of self-harm or hopelessness.
-
Combine therapy with lifestyle changes - CBT effectively addresses negative thought patterns while exercise, consistent sleep, and mindfulness accelerate recovery.
-
Early intervention prevents escalation - untreated situational depression can develop into clinical depression, but proper treatment typically leads to full recovery within months.
Remember, situational depression is a normal response to overwhelming life events, but it shouldn't be ignored. With the right support and treatment approach, most people not only recover but develop greater resilience for future challenges.
Introduction
Situational depression — it's a condition that affects roughly 10 percent of U.S. adults at some point in their lives, often appearing when life throws us a curveball that feels too big to handle. Have you recently gone through a major change and found yourself dealing with persistent sadness or feelings of hopelessness that seem to linger longer than expected?
You might notice yourself struggling with a low mood that just won't lift, unexpected crying spells, or finding it hard to enjoy the activities and relationships that used to bring you joy. The good news? These signs of situational depression typically start to improve within six months once the stressor has passed. However, when left untreated, situational depression can potentially develop into something more serious — clinical depression. While situational depression usually doesn't require medication for treatment, it's still a condition that deserves attention, as it's associated with an increased risk for suicide.
Understanding what situational depression looks like and recognizing the warning signs can make all the difference in your recovery. We'll explore what sets this condition apart from clinical depression, the subtle signs you shouldn't dismiss, and the effective strategies that can help you navigate this challenging period in your life.
What Is Situational Depression?
Feeling deeply sad after a difficult life event is completely natural, but sometimes these emotions can become overwhelming and start interfering with your daily life. Situational depression develops when your emotional response to a stressful event becomes excessive and begins disrupting your ability to function normally.
How it differs from clinical depression
Understanding the difference between situational and clinical depression can be important for finding the right support. Situational depression is directly tied to specific stressors or traumatic events, while clinical depression (major depressive disorder) can appear without any obvious trigger. Clinical depression tends to last longer and involves more severe symptoms that significantly impact sleep, eating habits, relationships, and poses a higher suicide risk.
While the symptoms might feel similar, situational depression is your mind's direct reaction to an identifiable event rather than stemming from biological or genetic factors. Remember, untreated situational depression can potentially develop into clinical depression if it continues without proper attention.
Why it's also called adjustment disorder
Mental health professionals often use the formal term "adjustment disorder with depressed mood" when diagnosing this condition. This name makes sense because the condition represents an excessive reaction to stress — one that involves negative thoughts, intense emotions, and behavioral changes that are much stronger than what we'd typically expect.
For a diagnosis to be made, symptoms must appear within three months of the triggering event, the stress you're experiencing must feel disproportionate to what happened, and there must be noticeable disruptions in your relationships and performance at work or school.
How long does situational depression last?
The timeline for situational depression varies from person to person. Most people experience symptoms anywhere from a few weeks to several months. According to diagnostic guidelines, symptoms typically show up within three months of the stressful event and last no longer than six months after the stressor has ended.
Several factors influence how long your symptoms might persist, including your family history, any underlying mental health conditions, and how severe the triggering event was. When the stressor continues over time — such as ongoing unemployment — adjustment disorders can extend beyond six months.
What Is Situational Depression?
Feeling deeply sad after a difficult life event is completely normal, but sometimes these feelings become more than we can manage. Situational depression occurs when your emotional response to a stressful event becomes so intense that it starts interfering with your daily life and activities.
How It Differs From Clinical Depression
There's an important distinction between situational depression and clinical depression that can help you understand what you're experiencing. Situational depression is directly tied to specific stressors or traumatic events, while clinical depression (major depressive disorder) can appear without any clear trigger. Clinical depression tends to last longer and involves more severe symptoms that significantly affect your sleep patterns, eating habits, and relationships, and it carries a higher suicide risk .
While the symptoms might feel similar, situational depression is your mind's direct reaction to an identifiable event rather than stemming from biological or genetic factors . Remember, untreated situational depression can potentially develop into clinical depression if it continues without proper care .
Why It's Also Called Adjustment Disorder
Mental health professionals use the formal term "adjustment disorder with depressed mood" when diagnosing situational depression . This name exists because the condition represents an excessive reaction to stress that involves negative thinking patterns, intense emotions, and behavioral changes that go far beyond what we'd typically expect .
For a diagnosis, your symptoms need to develop within three months of the triggering event, the stress you're experiencing must be disproportionate to what happened, and there must be significant disruptions in your relationships and performance at work or school .
How Long Does Situational Depression Last?
The timeline for situational depression varies from person to person. Most people experience symptoms lasting anywhere from a few weeks to several months . According to diagnostic criteria, symptoms typically emerge within three months of the stressful event and last no longer than six months after the stressor ends .
Several factors influence how long your symptoms might persist, including your family history, any underlying mental health conditions, and how severe the triggering event was . When the stressor continues (such as ongoing unemployment), adjustment disorders can last for more than six months .
Common Triggers and Risk Factors
Situational depression doesn't just appear out of nowhere. Certain events and personal factors can increase your risk of developing this condition. Understanding these triggers can help you recognize when you might be particularly vulnerable.
Major Life Changes Like Divorce or Job Loss
Life transitions often trigger situational depression, even when the changes seem positive. Divorce or relationship breakups can shake your emotional foundation, while job loss creates both financial stress and concerns about your identity and future. Retirement, moving for work or education, and having a baby all represent major life shifts that can trigger depressive symptoms.
Financial difficulties — including debt, unexpected medical expenses, or living paycheck-to-paycheck with unstable housing — create ongoing stress that can develop into situational depression. Work-related challenges, whether you're starting a new job or dealing with workplace conflicts, similarly add significant stress to your daily life.
Trauma and Unexpected Events
Traumatic experiences significantly increase your risk for situational depression. The death of a loved one, including beloved pets, can trigger intense grief that develops into adjustment disorder. Experiencing life-threatening situations — serious medical diagnoses, physical assaults, accidents, or natural disasters — often leave emotional scars that show up as depressive symptoms.
Being a victim of crime can also trigger situational depression, as can living in dangerous neighborhoods where safety concerns become a constant worry. These events can overwhelm your normal coping abilities, making it particularly difficult to adjust and move forward.
Family History and Past Mental Health Issues
Your genetic background plays a significant role in how vulnerable you are to depression. People with a first-degree family member who has experienced depression are 2.8-10 times more likely to develop depression themselves. This risk increases when multiple generations have been affected — grandchildren with two previous generations affected by depression face a three-fold increased risk of developing depression.
Past adverse childhood experiences, existing mental health conditions, and other stressful situations happening at the same time also increase your susceptibility. The relationship between your genetic makeup and environmental stressors creates a complex risk picture — someone with family history but excellent stress management skills may never develop depression, while those with both genetic predisposition and poor coping mechanisms face substantially higher risk.
Hidden Signs You Shouldn't Ignore
Spotting the early warning signs of situational depression isn't always straightforward, especially when you're already dealing with a challenging life situation. These symptoms often develop slowly and can easily be brushed off as normal stress responses. Let's explore the subtle indicators that deserve your attention.
Loss of interest in things you used to enjoy
Remember that hobby you used to look forward to every weekend? One of the most telling signs of situational depression is anhedonia — when activities that once brought you joy suddenly feel meaningless or exhausting. Maybe your weekly coffee dates with friends now feel like a chore, or that art class you loved attending seems pointless. This loss of interest often spreads beyond hobbies to affect your motivation at work or school, turning previously fulfilling tasks into empty obligations.
Persistent fatigue or sleep issues
Sleep problems are common companions of situational depression. You might find yourself tossing and turning at night, your mind replaying stressful events over and over. Or perhaps you're sleeping much more than usual but still waking up feeling drained. These disrupted sleep patterns create a challenging cycle — poor sleep makes it harder to cope with stress, which in turn makes sleep even more elusive.
Irritability or unexplained anger
Have you noticed yourself snapping at people over small things that wouldn't normally bother you? This unexpected irritability often signals that your emotional reserves are running low. You might feel constantly on edge or experience frustration that seems way out of proportion to whatever triggered it. This heightened irritability typically stems from being overwhelmed by significant stressors in your life.
Difficulty concentrating or making decisions
That mental fog you've been experiencing? It's another common sign of situational depression. Simple decisions can suddenly feel overwhelming, and focusing on everyday tasks becomes surprisingly difficult. You might find yourself reading the same paragraph multiple times, forgetting important details, or taking an unusually long time to make routine choices.
Withdrawing from social connections
Social withdrawal often happens gradually — first you decline a few invitations, then you start avoiding most social situations entirely. This isolation typically occurs at the exact time when you need support most, creating a counterproductive cycle that can deepen feelings of depression.
Thoughts of self-harm or hopelessness
The most serious warning sign involves persistent negative thoughts about yourself or the future. If you're feeling like things will never improve, that you're fundamentally flawed, or having any thoughts about death or self-harm, it's important to seek professional help immediately. These thought patterns indicate that situational depression has reached a critical stage requiring intervention.
Understanding these warning signs can help you recognize when it's time to seek support and take steps toward feeling better.
How to Deal with Situational Depression
Finding the right support for situational depression is an important step toward feeling better. While this type of depression might improve on its own once the stressor passes, getting proper help can speed your recovery and prevent it from developing into something more serious.
When to seek professional help
Professional help becomes necessary when your symptoms stick around for more than a few weeks, start interfering with your daily routine, or if you're having thoughts of self-harm. Remember, even though situational depression is usually temporary, it's still associated with increased suicide risk and shouldn't be brushed aside. If your symptoms continue for longer than 6 months after the stressful event has ended, clinical depression may be developing.
Situational depression treatment options
Treatment usually involves combining different approaches to find what works best for you. Mild cases might benefit from guided self-help and careful monitoring over 2-4 weeks. Moderate cases often respond well to therapy alone, while more severe symptoms might require both therapy and medication. Your healthcare provider will work with you to create a treatment plan that fits your specific situation and needs.
Therapy and counseling approaches
Cognitive Behavioral Therapy (CBT) can be particularly effective for situational depression because it helps you identify and change those negative thought patterns that keep you stuck. During CBT sessions, you'll learn to understand the connection between your thoughts and behaviors, focusing on practical ways to shift your thinking in the present moment. Interpersonal therapy takes a different approach by helping you improve communication skills in your relationships, while general counseling provides supportive guidance without telling you exactly what to do.
Lifestyle changes that help
Physical activity can make a real difference in how you feel — even a 30-minute daily walk has been shown to boost mood and energy levels. Establishing regular sleep and wake times helps your body regulate emotions more effectively, especially since sleep problems often make depression symptoms worse.
Eating regular, nutritious meals that include plenty of fruits, vegetables, whole grains, and lean proteins gives your brain the fuel it needs to support mental health recovery. Staying connected with friends and family is equally important, as is avoiding alcohol, nicotine, and drugs, which can interfere with your recovery process.
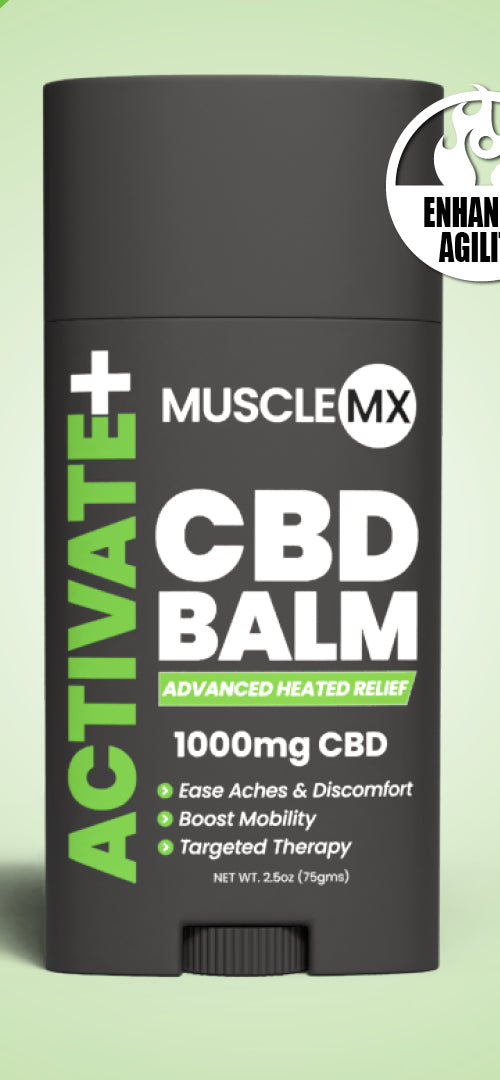
Can CBD for depression help?
Research on CBD for depression is still developing, but early findings show some promise. In one survey, approximately one in six people reported using CBD to manage depression, with two-thirds stating it worked moderately or very well. However, it's important to know that CBD products aren't regulated by the FDA (except for specific seizure medications), which means their contents and safety aren't always guaranteed.
Always consult with a healthcare provider before trying CBD, especially if you're taking other medications, as CBD can interact with certain drugs.
Using journaling and mindfulness techniques
Writing about your feelings and experiences can be a powerful tool for processing emotions and identifying what triggers your symptoms. Studies show that expressive writing actually reduces activity in the amygdala — the brain's emotion control center. You might try different approaches like expressive writing, gratitude journaling, or tracking your daily mood patterns.
Mindfulness meditation practices can help redirect your attention away from negative thinking patterns. Body scan meditation, sitting meditation, and walking meditation have all been shown to reduce depression symptoms by helping you stay focused on the present moment rather than getting caught up in worries about the future or regrets about the past.
Final Thoughts
Situational depression is more than just a temporary rough patch — it's a real condition that deserves understanding and care. We've explored how it differs from clinical depression, identified the warning signs that often get overlooked, and discussed the various approaches that can help you find relief.
Remember, recognizing these hidden signs early can be the difference between a manageable recovery and something more challenging down the road. Sleep disruptions, losing interest in things you once loved, persistent exhaustion, and that nagging irritability — these aren't just "normal stress responses" you should push through. They're your body and mind telling you it's time to seek support.
The path forward doesn't have to be overwhelming. Whether it's working with a therapist who specializes in cognitive behavioral techniques, making lifestyle adjustments that support your mental health, or exploring mindfulness practices that help you stay grounded, effective options exist. Professional guidance can make all the difference in how quickly and completely you recover.
You're certainly not alone in this experience. Situational depression affects roughly 10 percent of adults at some point in their lives, and many people find that with the right combination of support, self-care, and sometimes professional treatment, they can move through this difficult period. What's more, many individuals discover they emerge with greater resilience and a deeper understanding of their own strength.
Your healing journey is uniquely yours, and taking the first step toward getting help — whether that's reaching out to a counselor, talking to your doctor, or simply acknowledging that what you're experiencing matters — is already progress worth celebrating.
FAQ's about Situational Depression
Q: How can I tell if my situational depression is becoming clinical depression?
A: Situational depression may be evolving into clinical depression if symptoms persist for more than six months after the triggering event has ended, or if they significantly disrupt your daily functioning. Seek professional help if you experience severe symptoms or thoughts of self-harm.
Q: What are some common triggers for situational depression?
A: Common triggers include major life changes like divorce or job loss, traumatic events such as the death of a loved one, financial hardships, and unexpected life-threatening situations. Family history and past mental health issues can also increase susceptibility to situational depression.
Q: What are the hidden signs of situational depression I shouldn't ignore?
A: Watch for loss of interest in activities you once enjoyed, persistent fatigue or sleep issues, unexplained irritability or anger, difficulty concentrating, social withdrawal, and thoughts of hopelessness. These signs may develop gradually but shouldn't be dismissed.
Q: How is situational depression treated?
A: Treatment typically involves a combination of therapy (such as Cognitive Behavioral Therapy), lifestyle changes (like regular exercise and improved sleep habits), and in some cases, medication. The specific approach depends on the severity of symptoms and individual needs.
Q: Can lifestyle changes help with situational depression?
A: Yes, lifestyle changes can significantly help manage situational depression. Regular physical activity, maintaining a consistent sleep schedule, eating a nutritious diet, and practicing mindfulness techniques like journaling and meditation can all contribute to recovery and improved mental well-being.
References
https://www.meditelecare.com/situational-vs-clinical-depression-how-to-tell-the-difference/
https://www.healthline.com/health/depression/situational-depression
https://www.webmd.com/depression/situational-depression
https://medicine.umich.edu/dept/psychiatry/news/archive/202012/5-red-flags-youre-dealing-situational-depression
https://mentalhealth.banyantreatmentcenter.com/blog/situational-depression-symptoms-and-causes/
https://www.healthline.com/health/depression/situational-depression-vs-clinical-depression
https://www.mayoclinic.org/diseases-conditions/adjustment-disorders/symptoms-causes/syc-20355224
https://seaglassrecoveryarizona.com/what-is-situational-depression/
https://pmc.ncbi.nlm.nih.gov/articles/PMC3918432/
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2778480
https://www.premierhealth.com/your-health/articles/women-wisdom-wellness-/family-history-and-depression-what-s-the-link-
https://www.webmd.com/cannabinoids/cbd-depression-anxiety
https://therapyinanutshell.com/how-to-journal-for-anxiety-and-depression-6-ways-to-process-emotions-with-writing/