What Does Pain Management Do? Should I Do It?
|
| When you get a cut, scratch, bruise, or even a broken bone, even though the pain might be severe, you know it will get better with some time and rest. However, some conditions don’t simply get better but go on chronically, sometimes for years. |
Some illnesses and diseases cause pain that must be managed instead of cured. What are some of these conditions, and how can pain be managed?
What Are Some Methods of Managing Pain?
The first step in pain management is to talk to your doctor about your level of pain. If the pain you’re experiencing makes it difficult to do basic tasks, your pain management may be much more intensive, requiring surgery, strong medication, or physical therapy.
If your pain is annoying or aggravating but not debilitating, simple home remedies may be enough to manage your pain. Let’s look at some common methods for managing pain and some strategies you can try at home.
A pain management specialist may recommend any of the following options for managing your pain, depending on the cause and the severity:
Medications
Depending on the source of the pain, there are several medications that may help manage your pain. Some medications have significant side effects, so it’s important to make sure that the benefit outweighs the cost.
Some of these medications include:
-
NSAIDs (non-steroidal anti-inflammatory drugs): These medications work by reducing inflammation in the body, which can help lessen pain. NSAIDs like ibuprofen are available over-the-counter, but a doctor can prescribe a higher dose if needed.
-
Prescription pain medication: If the pain is intense enough, your doctor may prescribe opiate medication. Usually, these drugs are combined with acetaminophen to help treat pain, while opiate medication affects the brain’s perception of pain.
-
Muscle relaxers: These medications are depressants that affect the central nervous system. They have a sedating effect and can cause sleepiness, but they also block pain sensations.
-
Nerve pain medications: Gabapentin and similar medications work by subduing the pain receptors in the brain that sense nerve pain, especially from conditions like neuropathy. Often nerve pain medications are also used as antidepressants.
Injections
If there’s a specific area of pain, like a joint or muscle, then one option for pain management might be an injection of steroids or another formula to lessen inflammation or block nerve pain sensors.
It’s common for those who struggle with lower back pain to receive injections at the site of a damaged spinal disc of steroids that can eliminate or lessen pain for weeks, months, or even years. Those with chronic migraine headaches can receive a botox injection to keep the headaches away.
Surgical Procedures
Usually, having surgery is considered a last resort, but severe conditions might make an operation necessary to manage pain. For example, if you have a ruptured disc in your back, it may be necessary to surgically repair the disc so it’s no longer pressing on a nerve. Life-threatening conditions that cause severe pain, like cancer, often also require surgery.
Physical Therapy
 If you’re dealing with a physical injury like a broken bone, muscle tear, or dislocated joint, a physical therapist may be recommended to help you manage your pain. Physical therapists can work with you to strengthen areas of your body that have become weak from injury, and they can teach you exercises you can do at home to maintain your mobility and keep from reinjury.
If you’re dealing with a physical injury like a broken bone, muscle tear, or dislocated joint, a physical therapist may be recommended to help you manage your pain. Physical therapists can work with you to strengthen areas of your body that have become weak from injury, and they can teach you exercises you can do at home to maintain your mobility and keep from reinjury.
Often physical therapists have access to TENS (transcutaneous electrical nerve stimulation), which are electrodes connected to an area of pain and deliver low-level shocks designed to confuse pain signals and give you relief.
Changes in Lifestyle
Sometimes simple changes in your routine or habits can be the most important factors in your pain management. Issues with weight management, drinking too much alcohol, and smoking can cause pain issues to worsen and cause other problems to arise.
Diet and exercise can also affect pain levels, and a nutritionist can give you insight into how to eat for pain management.
Heat and Ice
One of the easiest ways to calm pain is by applying either heat or cold. If you’re dealing with tense, painful muscles, then a warm bath, jacuzzi or hot compress can provide soothing. If you’re experiencing an inflamed joint, applying an ice pack might be a good way to reduce pain.
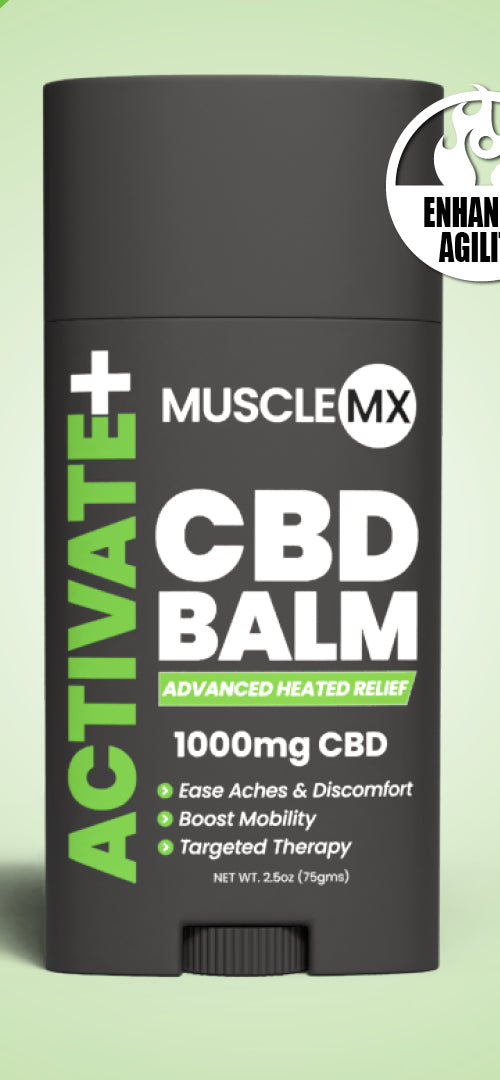
Topical Rubs
If a specific area is causing you pain, you can use creams, lotions, balms, and oils that target pain. Some pain topicals work by confusing your nerves (for example, topicals made from hot chili peppers), while others use medicines like lidocaine to numb the area of pain. Natural products use herbs and plants to ease tension and relax muscles.
What Are the Different Types of Pain?
Different types of pain may require different kinds of pain management. Pain is categorized by how long it affects, what it feels like, and what’s causing it. Some pain is the result of an injury or disease, while other pain occurs because the body's nerves are damaged and aren’t working properly. Let’s take a look at some of the main types of pain:
Acute vs. Chronic Pain
One way to classify pain is by how long it affects you. Acute pain can hurt a lot but starts to get better right away. Injuries like strains, sprains, gashes, cuts, and bruises are all examples of acute pain because they immediately start healing. Acute pain is short-term. Unless you have an extremely traumatic injury or illness, you probably won’t experience it for a long period of time.
If you’re dealing with acute pain, then you might describe it as:
- Stabbing
- Sharp
- Shooting
- Throbbing
- Intense
Chronic pain is different because it goes on for an extended period of time. Often it won’t get better on its own, so it’s one of the main categories where pain management is needed. Lower back pain, irritable bowel syndrome, arthritis, and diabetes are all conditions that cause chronic pain. The discomfort might be gnawing, throbbing, or pulsating, and it may feel similar to acute pain.
Nociceptive Pain
Any pain directly resulting from damage to the body tissue is considered nociceptive.
There are two main types of nociceptive pain:
-
Somatic: When the bone, muscle, or skin tissue is affected, then you experience somatic pain. This is what you feel when you are physically injured with a wound, broken bone, or pulled muscle. Somatic pain usually feels very intense, but like acute pain, it often gets better with a little time.
-
Visceral: When the internal organs are damaged, then the pain will be visceral. This type of pain is often described as pressing, squeezing, or aching. Stomach aches, discomfort in the chest and lungs, or menstrual cramps are all examples of visceral pain.
Both types of nociceptive pain might require pain management depending on what’s causing it and how severe it is.
Neuropathic Pain
One of the most difficult types of pain to diagnose, treat, and manage is neuropathic pain. Neuropathic conditions are associated with damage to the central nervous system. When the nerves in the body are damaged, they send conflicting, confused messages to the brain.
Often, this nerve confusion causes aching, burning, numbness, or even electrical-like pain, often in the hands, feet, legs, arms, neck, or back.
What Conditions Might Require Pain Management?

Any physical condition that includes persistent pain could require pain management. If you suffer from chronic pain, then this will be very important! Here are some of the major conditions where pain management is necessary:
Neuropathy
A common symptom of diabetes, neuropathy is caused by damage to the central nervous symptom. If you suffer from neuropathy, you’ll usually feel tingling, burning, and often throbbing/aching hands and feet. It can be difficult to figure out the triggers of neuropathy, and it may often be felt in flare-ups that come and go. It can be extremely uncomfortable, and because it isn’t curable, the pain must be managed.
Fibromyalgia
An autoimmune disorder, there’s still a lot that isn’t known about fibromyalgia. It affects the central nervous system and causes severe fatigue, body aches, and recurring headaches. Because people with fibromyalgia may have cycles of symptoms, pain management is crucial to being able to live a normal life.
Migraine Headaches
There are very few common physical problems as debilitating as migraine headaches. These intense headaches can come without warning, often from a particular trigger. If you get a migraine, you may not be able to do anything but wait for it to pass, which, in more severe cases, can take days. Managing the pain a migraine brings is vital.
Sickle Cell Anemia
A genetic condition, sickle cell anemia causes the body's blood cells to become abnormally formed. It can be an extremely painful condition for which there is no cure. Pain management is the only treatment for sickle cell anemia.
Sciatica
When the discs in the spinal cord are pressed, pinched, slipped, or ruptured, this puts pressure on the nerves that connect the rest of the body to the spinal cord. Sciatica is pain from pressure on the sciatic nerve (one of the nerves in the back). Sciatic pain can be felt from the lower back to the feet. Surgery might be required in severe cases, but pain management and physical therapy can often improve sciatica.
Arthritis
Any condition with an “-itis” is an inflammatory condition. Arthritis is when one or more joints in the body become inflamed. There are many different types of arthritis, with osteoarthritis, rheumatoid arthritis, and gout being some of the most common. Some arthritis conditions aren’t reversible or curable, so the only treatment is to manage the pain and flare-ups when they come.
Managing Your Pain
If you’re currently dealing with debilitating, chronic pain, talk to your healthcare provider about how you can improve your symptoms to live a more mobile and active life.
If you have nagging pain that’s annoying but not necessarily debilitating, consider trying some of the home remedies for pain management. Start managing your pain so that it doesn’t manage you.
Sources:
Transcutaneous electrical nerve stimulator (TENS) | University of Iowa Hospitals & Clinics
Peripheral Neuropathy | National Institute of Neurological Disorders and Stroke
Gabapentin: Uses, Side Effects, Dosages, Interactions & More | Cleveland Clinic






























 If you’re dealing with a physical injury like a broken bone, muscle tear, or dislocated joint, a physical therapist may be recommended to help you manage your pain. Physical therapists can work with you to strengthen areas of your body that have become weak from injury, and they can teach you exercises you can do at home to maintain your mobility and keep from reinjury.
If you’re dealing with a physical injury like a broken bone, muscle tear, or dislocated joint, a physical therapist may be recommended to help you manage your pain. Physical therapists can work with you to strengthen areas of your body that have become weak from injury, and they can teach you exercises you can do at home to maintain your mobility and keep from reinjury.