What Is Pain Management? Understanding Your Pain Treatment Plan
|
| Pain is an experience that affects everyone at some point in our lives. And just as the weather can be unpredictable and volatile, pain can also be relentless and unwavering. Imagine being stuck in a storm of pain, unable to find shelter and escape its effects. It’s unpleasant, but not all hope is lost. |
Managing pain is like navigating through a storm — you need a map, a compass, and a sturdy vessel. That's where pain management comes in. Pain management is the umbrella term for the various strategies and treatments to alleviate or minimize pain. From pain medicines and physical therapy to acupuncture and lifestyle changes, there are many tools in the pain management arsenal.
This article will provide an overview of the different types of pain, the various treatment options available, and the steps you can take to develop an effective pain treatment plan. So, let's set sail on our journey toward pain management and better quality of life.
How Does Pain Work?

To understand pain management, it is crucial first to understand pain itself. Pain can be broadly categorized into two types: acute and chronic. Acute pain is short-lived, sharp, and intense pain resulting from an injury or surgery. It serves as an alarm signal, warning us of potential harm and prompting us to take action to prevent further damage.
Chronic pain, on the other hand, is persistent pain lasting more than three months. Chronic pain can stem from various conditions, including arthritis, low back pain, fibromyalgia, and neuropathic pain.
With chronic pain, the alarm signal fails to shut off, and the underlying cause is often challenging to identify. In fact, chronic pain has birthed an entirely new area of medical study known as the biopsychosocial model of pain.
The Biopsychosocial Model of Pain
Imagine you have a friend struggling with a persistent ache in their back for months. They've seen numerous doctors, undergone multiple tests, and tried various treatments, but nothing seems to provide lasting relief. As a result, they feel frustrated and hopeless.
From a biopsychosocial perspective, their back pain isn't just a physical problem; it's also a psychological and social one. The psychological component considers how the patient's thoughts and beliefs affect their pain perception. For example, if they are feeling hopelessness or experiencing depression, they may experience more intense or longer-lasting pain.
The social component, meanwhile, looks at the role of interpersonal and environmental factors in influencing pain.
Do they feel supported? Are specific stressors, such as financial difficulties or relationship issues, making it harder for them to cope with their pain? The biopsychosocial model recognizes that each patient's experience of pain is unique and requires a personalized approach to treatment.
Once a healthcare provider knowledgeable in pain management has identified the underlying cause of an individual's pain, they can develop a customized treatment plan that takes into account both the physical and psychosocial components of pain.
What Healthcare Providers Can Address Pain?
In the world of pain management, many different players can help alleviate suffering. Healthcare providers, such as pain management specialists, anesthesiologists, neurologists, pharmacists, and chiropractors, are all key pain management team members.
Each of these experts brings unique skills and tools to the table, allowing them to address different aspects of the pain experience.
Pain Management Specialists
Pain management specialists are medical doctors trained in diagnosing and treating pain. They work with patients to develop personalized pain treatment plans, combining medication, interventional procedures, and physical therapy, if needed. These specialists play a crucial role in managing chronic pain, acting as guides and partners in the quest for relief.
Anesthesiologists
Anesthesiologists are medical doctors who specialize in managing pain during and after surgical procedures. However, they are not limited to the operating room and can significantly manage chronic pain. Anesthesiologists often use nerve blocks, epidural steroid injections, and spinal cord stimulation to relieve pain. In addition, they work hand-in-hand with pain management specialists to develop a comprehensive pain treatment plan.
Neurologists
Neurologists are medical doctors who specialize in treating conditions related to the nervous system. They often work with patients who have chronic pain due to conditions like neuropathic pain, fibromyalgia, and shingles. Neurologists can also play a crucial role in the management of cancer pain. They often work with pain management specialists to develop a treatment plan that addresses the underlying cause of pain.
Pharmacists
Pharmacists play an essential role in pain management by helping patients understand their medications, their side effects, and any potential interactions with other medicines. Pharmacists can also guide over-the-counter pain medications and how they can be used in combination with prescription medications. In addition, they work closely with other healthcare providers to ensure that patients receive safe and effective pain relief.
Chiropractors
Chiropractors specialize in treating musculoskeletal conditions and pain. They often use spinal manipulation and other manual therapies to relieve pain in the neck, back, and other body parts. Chiropractors may also guide lifestyle changes that can help manage chronic pain, working in partnership with other healthcare providers to develop a comprehensive pain treatment plan.
What Medications Are Used To Manage Pain?

Medications can often play a crucial role in managing pain, and in this section, we will delve into some of the most commonly used options for alleviating discomfort.
From drugs that interact with the central nervous system to over-the-counter remedies, we will explore the physiological mechanisms behind each and how they work to soothe the aches and pains of the human body.
Over-the-Counter Medications
In the face of persistent pain, many individuals seek out over-the-counter medications as a means of relief and pain control. These drugs, which can be purchased without a prescription, offer a quick solution for those in pain.
However, it's important to note that over-the-counter medications do not address the root cause of the pain. For instance, chronic pain will generally not be resolved by taking nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen.
These drugs work by blocking the production of pain-causing chemicals in the body, such as prostaglandins, or by providing a short-term boost of pain-relieving substances, such as acetaminophen. By doing so, over-the-counter medications can offer a brief respite from discomfort and help to improve quality of life and mental health.
Muscle Relaxants
These drugs affect the communication between nerve cells, specifically by inhibiting the release of the neurotransmitter acetylcholine. By blocking the signaling of acetylcholine, muscle relaxants help to reduce muscle tension, spasms, and pain. Some of the most commonly used muscle relaxants include cyclobenzaprine and carisoprodol.
Antidepressants
Antidepressants, such as amitriptyline and nortriptyline, are often prescribed for their pain-relieving effects, even when depression is not present. Broadly, they target the neurotransmitters serotonin and norepinephrine, which regulate mood and pain perception.
By increasing the levels of these neurotransmitters in the brain, antidepressants help to reduce chronic pain and improve overall mood. However, as discussed, pain is a biopsychosocial phenomenon, so it's essential to consider pain management's physical and psychological aspects.
Opioids
When it comes to managing pain, opioids are often considered a last resort. These powerful drugs have the potential for significant side effects and are often associated with the opioid epidemic.
Despite this, they can effectively treat severe, chronic pain when all other options have failed. However, it is important to use caution and follow the guidance of a healthcare provider when considering opioid use for pain management.
What Are Interventional Procedures for Pain Relief?
When medication and lifestyle changes aren't enough to manage pain, individuals may turn to interventional procedures or complementary therapies for relief.
These options provide a more direct approach to alleviating discomfort and can be tailored to each individual's specific needs:
-
Nerve Blocks: Nerve blocks are like a roadblock for pain signals, effectively blocking their transmission by injecting a local anesthetic. By doing so, individuals can experience temporary relief from chronic headaches, neck pain, and low back pain.
-
Spinal Cord Stimulation: Imagine a device that acts like a traffic cop, directing pain signals down a different path. That's the idea behind spinal cord stimulation, a procedure that uses electrical impulses to block the transmission of pain. This procedure can be a game-changer for those with chronic pain conditions like failed back syndrome or complex regional pain syndrome.
-
Radiofrequency Ablation: This minimally invasive procedure is like a heat-seeking missile, targeting and destroying tiny nerve fibers that transmit pain. By doing so, individuals with conditions like arthritis or neck pain can experience significant relief.
-
Epidural Steroid Injections: Picture a soothing balm for inflamed nerves. That's what epidural steroid injections can provide, with a corticosteroid injected into the area surrounding the spinal cord. This procedure can help reduce inflammation and relieve pain in the lower back, neck, and legs.
How Can Physical Therapy Address Pain?

Above all else, physical therapy is a remarkable way to manage pain that involves exercise and movement to help you feel better. It's not a quick fix, like taking a pain reliever, but a way to address the root cause of your pain and help you live a life free from discomfort.
Whether you're dealing with chronic pain, arthritis, or recovering from an injury, physical therapy can be a valuable ally on your journey to a pain-free life. By focusing on the underlying cause of your pain and helping you build strength, physical therapy can give you the tools you need to take control of your discomfort and live your best life.
To effectively manage pain, it's essential to embark on a comprehensive and holistic journey that begins with creating a pain treatment plan.
This plan should encompass a thorough assessment of pain conditions, including carefully evaluating available treatment options, considering potential side effects and risks, implementing important lifestyle changes, and open and ongoing communication with healthcare providers.
By taking a well-rounded approach, individuals can chart a course toward finding the right combination of treatments to manage their pain and improve their quality of life in meaningful ways.
The Bottom Line
Pain management can be a journey, but it doesn't have to be a struggle. By taking a well-rounded approach and considering all options, from medication to physical therapy, you can find the right combination of treatments to improve your quality of life.
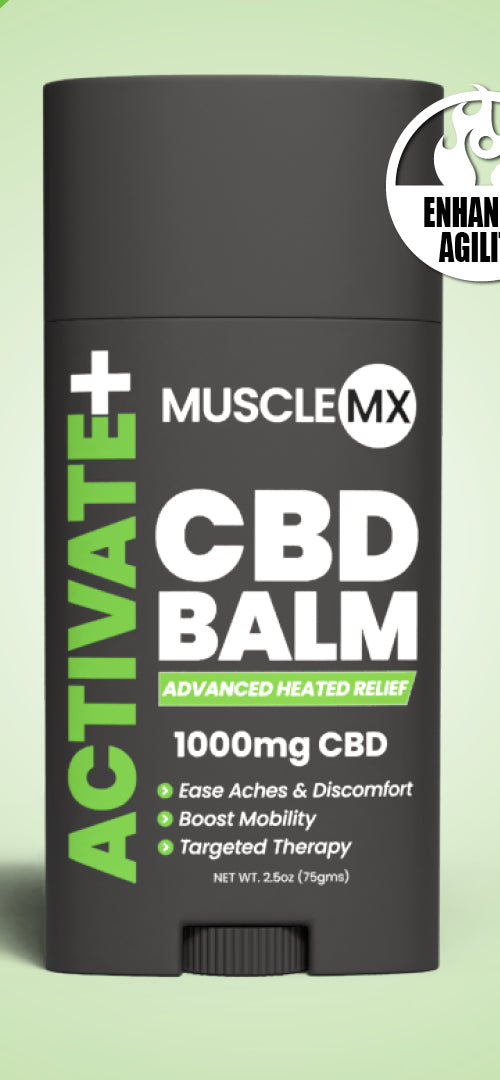
At Muscle MX, we believe in combining modern science with traditional remedies to help you feel your best and live an active, healthy life. Let's work together to make comfort and well-being the norm.
Sources:
Antidepressants: Another weapon against chronic pain | Mayo Clinic
The Biopsychosocial Approach | Journal of Practical Pain Management
Muscle Relaxers: What They Are, Uses, Side Effects & Types | Cleveland Clinic