Does Ice Really Reduce Swelling? What Medical Experts Want You to Know
Does ice reduce swelling? This age-old remedy, trusted by athletes and medical professionals alike, might not be as straightforward as we once thought. While reaching for an ice pack after an injury seems instinctive, recent research has sparked debate about its effectiveness. Many are now asking, "Does ice actually help?"
For decades, the RICE method (Rest, Ice, Compression, Elevation) has been the gold standard for injury treatment. However, emerging studies suggest that our body's inflammatory response serves a crucial purpose in healing. Understanding when to use ice - and when to explore alternatives like a cbd cooling balm or other athletic recovery methods - can significantly impact your healing process.
This comprehensive guide examines the science behind ice therapy, separates fact from fiction, and provides expert-backed recommendations for managing swelling effectively. We'll explore why ice helps swelling and whether icing actually helps injuries, giving you a clearer picture of this common treatment method.
The Science Behind Ice and Inflammation
Understanding inflammation helps explain why ice's role in injury treatment remains debated among medical experts. The body's inflammatory response, far from being harmful, serves as a crucial first step in the healing process [1].
How inflammation works in the body
Inflammation begins immediately after injury when the immune system dispatches white blood cells and specialized chemicals to the affected area [2]. This natural defense mechanism triggers several visible signs:
-
Redness and warmth from increased blood flow
-
Swelling from fluid accumulation
-
Pain from nerve stimulation
-
Reduced range of motion
These symptoms, although uncomfortable, indicate that healing has begun [1]. Specifically, inflammatory cells release insulin-like growth factor (IGF-1), which primarily drives tissue repair [3]. The lymphatic system plays a crucial role in this process, helping to remove waste products and excess fluid from the injured area.
What happens when we apply ice
When ice contacts injured tissue, it creates several immediate physiological changes [4]. The cold temperature reduces nerve activity and lowers skin temperature, consequently decreasing pain sensation [4]. Furthermore, ice acts as a vasoconstrictor, limiting blood flow to the injured area [3]. This vasoconstriction is a key factor in why ice helps swelling, as it reduces the amount of fluid accumulating in the injured tissue.
Latest research findings
Recent studies have challenged traditional beliefs about icing injuries. Notably, research indicates that prolonged ice application can actually delay healing by interfering with the body's natural inflammatory response [3]. The cold creates a roadblock for white blood cells attempting to reach the injured area [5], potentially hindering the process of phagocytosis, where these cells engulf and remove damaged tissue.
Scientists have discovered that inflammation, despite being uncomfortable, plays an essential role in muscle regeneration after acute injuries [5]. In fact, a lack of inflammation can lead to poor muscle recovery [5]. This understanding has prompted many medical experts to reconsider when ice therapy should be used.
The timing of ice application particularly matters. Studies show that while ice can help manage severe swelling, it may impede recovery in cases where edema levels are not significant [3]. Additionally, prolonged ice exposure risks tissue damage and potential nerve complications [3].
These findings suggest that although ice remains valuable for pain management, its traditional role in injury treatment requires careful consideration. The key lies in understanding when swelling reduction benefits outweigh the potential delay in natural healing processes. This has led to the question: does ice help with inflammation in all cases, or are there times when it might be counterproductive?
Common Myths About Ice Therapy
Traditional beliefs about ice therapy have undergone substantial scrutiny in recent years, prompting medical experts to reassess long-held practices.
The RICE method controversy
The RICE protocol, introduced in 1978, stood unchallenged as the gold standard for injury treatment [6]. Moreover, this approach gained widespread acceptance among clinicians, trainers, and physical therapists. Subsequently, Dr. Gabe Mirkin, the creator of RICE, made a surprising announcement in 2015 - he recanted his support for the protocol [6].
Research has revealed that ice application can actually impede the healing process [6]. As a result, studies show that using ice on acute injuries creates a hypoxic environment, leading to cell death [6]. This discovery has prompted a shift away from automatic ice application for every injury, raising the question: is icing bad for healing in some cases?
Is complete swelling reduction good?
One of the most persistent myths suggests that all swelling needs immediate reduction. Primarily, this belief stems from outdated understanding of the healing process. The truth presents a more nuanced picture:
-
Swelling serves as the body's natural first response to injury [7]
-
The inflammatory process sends essential macrophages and white blood cells to repair damaged tissue [7]
-
Complete swelling prevention can interrupt the body's natural healing sequence [7]
The body's inflammatory response essentially acts as an internal repair crew. When we apply ice to reduce all swelling, we inadvertently restrict blood vessels, allowing less fluid to reach the injured area [7]. This narrowing of blood vessels persists even after ice removal, continuing to delay the natural healing process [7].
Medical research indicates that while excessive swelling can impede recovery, some level of inflammation proves beneficial [8]. The key lies in understanding when swelling reduction truly helps versus when it hinders healing. For instance, ice might benefit cases with severe joint sprains where too much prolonged swelling could slow recovery [8].
Athletic recovery methods have evolved beyond the simplistic "ice-everything" approach. Modern treatment protocols recognize that while ice can provide temporary pain relief [9], its use should be strategic rather than automatic. This understanding has led to more nuanced approaches, including the selective use of cbd cooling balm and other targeted recovery techniques when appropriate.
When Ice Actually Works
Clinical evidence supports specific scenarios where ice therapy proves beneficial for injury management. Primarily, ice treatment shows effectiveness in acute soft tissue injuries, where it can reduce pain and control excessive swelling [8]. But how does ice help healing, and when is it most effective?
Acute injury scenarios
Ice therapy demonstrates particular effectiveness for several types of injuries. Initially, minor ligament sprains around joints like knees, wrists, or ankles respond well to cold therapy [8]. During muscle injuries, ice application helps reduce muscle spasms and ease soreness [8]. Accordingly, tendon injuries benefit from cold treatment through decreased prostaglandin E2 production, which directly impacts pain reduction [8].
Cold therapy can be particularly helpful in managing tendonitis, a common overuse injury. The analgesic effects of ice can provide relief from the pain and inflammation associated with this condition.
Optimal timing for ice application
The timing of ice application plays a crucial role in its effectiveness. Generally, ice therapy yields the best results within the first 72 hours after an injury occurs [1]. But does ice help swelling after 3 days? While it may still provide some benefit, its effectiveness tends to decrease after this initial period. For maximum benefit:
-
Apply ice for 15-20 minutes at a time [2]
-
Allow 30-40 minutes between applications [2]
-
Continue treatment as needed while monitoring skin response [10]
Ice treatment should begin as soon as possible after injury [10]. Therefore, keeping ice packs readily available, especially in athletic settings, enables prompt treatment [11]. Soon after an acute injury, such as an ankle sprain, immediate ice application can reduce long-term swelling and potentially decrease recovery time [11].
Signs ice is helping
Undoubtedly, proper ice application produces noticeable effects that indicate its effectiveness. The treatment works correctly when:
-
Pain levels decrease through numbing of the affected area [9]
-
Visible reduction in swelling occurs [9]
-
Bleeding in the injured area diminishes [9]
-
Muscle spasms decrease [8]
Ice therapy remains most effective for managing acute injuries where inflammation control is crucial [12]. For chronic conditions, ice may still prove beneficial when applied after activities to help control inflammation, though never before exercise [12].
Remember that while ice helps reduce pain and swelling, it doesn't accelerate healing [10]. The goal focuses on managing symptoms and preventing excessive swelling that could impede recovery [8]. If swelling persists beyond 48 hours, this might indicate a more serious injury requiring professional evaluation [2].
When Ice May Harm Recovery
Recent medical research reveals crucial distinctions between beneficial and potentially harmful ice therapy applications. Understanding these differences helps prevent complications and ensures optimal recovery outcomes. But does ice slow down healing in some cases?
Types of injuries to avoid icing
Certain injuries and conditions make ice therapy inadvisable or even dangerous. Primarily, muscle tears with minimal swelling should avoid ice application, since cold therapy might act as a barrier to recovery [8]. Indeed, prolonged cold exposure leads to reduced blood flow, potentially causing tissue death or permanent nerve damage [8].
Medical experts caution against using ice therapy for:
-
Chronic pain conditions
-
Regenerating peripheral nerve injuries
-
Open wounds or infections
-
Restricted range of motion due to scar tissue
-
Injuries requiring immediate muscle repair
-
Areas with impaired circulation
Likewise, individuals with specific medical conditions face heightened risks from ice therapy. These include those with hypertension, Raynaud's disease, rheumatoid arthritis, local limb ischemia, or previous frostbite injuries [13].
Warning signs to watch for
Recognizing adverse reactions to ice therapy remains crucial for preventing complications. A prolonged period of cold application creates a hypoxic environment, causing cell death [6]. Henceforth, patients should immediately discontinue ice therapy upon experiencing:
First, skin changes warrant attention - watch for unusually firm or waxy skin texture, plus any discoloration turning white or grayish-yellow [14]. Next, monitor for signs of nerve involvement, including persistent numbness or tingling sensations that don't resolve quickly after removing ice [14].
Physical symptoms requiring immediate ice removal include excessive shivering, unusual exhaustion, or declining energy levels [14]. Furthermore, cognitive changes like confusion, slurred speech, or memory problems indicate potential complications from prolonged exposure [14].
Conventional cold therapy often leads to extended application periods, risking serious side effects including nerve injuries, healing process restrictions, and neuromuscular impairments [8]. Most concerning, ice application can prevent the body's natural release of IGF-1, thereby delaying the start of healing and recovery [8].
For athletes and active individuals, applying ice immediately prior to physical activities presents additional risks. This practice frequently leads to muscle and joint stiffness, potentially increasing injury susceptibility [15]. Instead, alternative recovery methods like cbd cooling balm might offer safer options for pre-activity preparation.
It's important to note that nerve damage from icing too long is a real concern. Prolonged exposure to cold can cause temporary or even permanent damage to superficial nerves, leading to numbness, tingling, or loss of sensation in the affected area.
Expert-Recommended Ice Application Methods
Medical professionals have established precise protocols for ice therapy application, ensuring both safety and effectiveness. Proper technique makes a significant difference in treatment outcomes. Understanding what does icing an injury do and how to apply it correctly is crucial for optimal results.
Direct vs indirect application
Proper ice application requires careful consideration of the method used. Primarily, two approaches exist: direct and indirect application. Direct application involves placing ice in direct contact with the affected area, whereas indirect methods use barriers between ice and skin [16].
A thin barrier, namely a washcloth or paper towel, must always separate ice from skin to prevent tissue damage [17]. Alternatively, crushed ice or frozen gel packs offer superior molding capabilities around injured areas [3]. For those with sensitive skin, dampening the protective barrier can speed up the cooling process while maintaining safety [18].
Duration guidelines
Current medical research firmly establishes optimal icing durations. The maximum recommended time for any ice application stands at 20 minutes [5]. Extending beyond this timeframe triggers reactive vasodilation - a counterproductive widening of blood vessels that undermines the treatment's benefits [3].
The body provides clear signals during proper ice application through the CBAN method:
-
Cold: Initial sensation upon application
-
Burning: Brief stinging feeling follows
-
Aching: Development of dull discomfort
-
Numbness: Signal to remove ice [1]
Frequency recommendations
Proper timing between ice applications proves crucial for optimal results. Medical experts recommend waiting 30-40 minutes between sessions [5]. This interval prevents tissue damage while maintaining therapeutic benefits. Furthermore, spacing sessions allows the body to reset its natural responses [3].
For acute injuries, experts suggest following this schedule:
-
Begin treatment within first 24-48 hours
-
Apply ice for 20 minutes
-
Wait minimum 30 minutes between applications
-
Continue as needed while monitoring skin response [19]
Presently, research indicates that ending treatment cycles with ice proves most beneficial, unless treating chronic back spasms [5]. This approach helps maintain reduced inflammation levels by keeping blood vessels constricted. Hence, timing becomes crucial - applying ice immediately after injury yields maximum benefits [3].
Evidence suggests that proper ice application can match or exceed the effectiveness of oral medications and injections when used correctly [5]. Currently, medical professionals emphasize the importance of consistent monitoring during treatment. Evidently, successful outcomes depend on adhering to these expert-recommended protocols while remaining attentive to body responses throughout the treatment process.
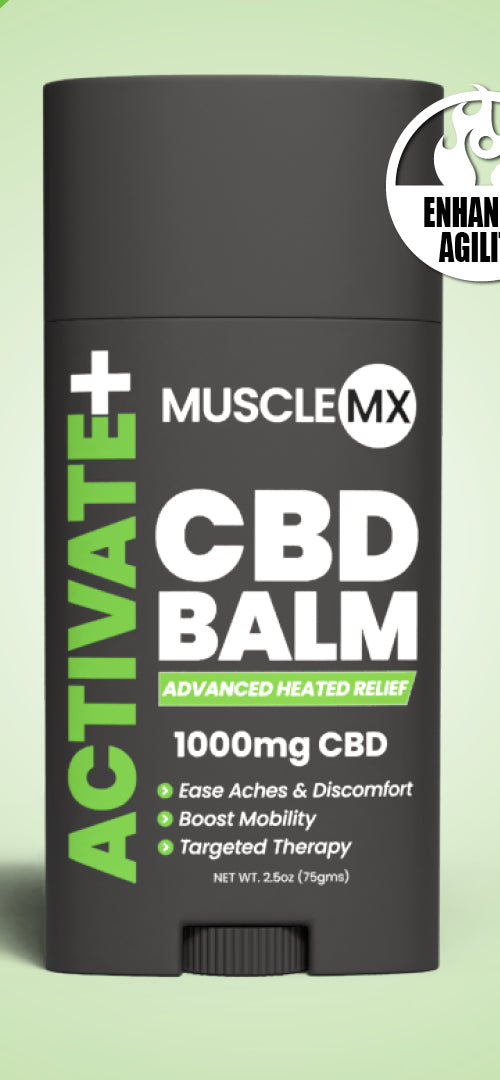
CBD Cooling Balm
Muscle MX Recovery CBD Balm offers a compelling alternative to traditional ice therapy for pain and swelling, or it can be used in conjunction with it for enhanced results. Unlike ice, which primarily focuses on reducing inflammation through cold application, the balm harnesses the power of all-natural ingredients, including CBD, to provide a holistic approach to recovery. The CBD in the balm interacts with the body's endocannabinoid system, potentially reducing pain and inflammation more effectively than ice alone. Additionally, the balm's natural ingredients, such as essential oils and plant extracts, nourish the skin and promote healing, making it a versatile option for those seeking a natural, soothing remedy for muscle recovery.
Conclusion
Medical understanding of ice therapy has evolved significantly from the traditional "ice everything" approach. While ice remains valuable for acute injury management, its application requires careful consideration of timing, injury type, and individual circumstances.
Research clearly shows that some inflammation serves a vital purpose in healing. Therefore, strategic ice application proves most beneficial during the first 72 hours after injury, particularly for acute soft tissue injuries with excessive swelling. However, automatic ice application for every injury might delay natural healing processes.
Successful ice therapy depends on proper technique and timing. Following expert guidelines - 20-minute applications with adequate rest periods - helps maximize benefits while avoiding potential complications. Additionally, watching for warning signs and stopping treatment when numbness occurs ensures safe, effective recovery.
The key takeaway reflects a balanced approach: ice therapy works best as part of a thoughtful treatment strategy rather than a universal solution. Medical experts now recommend evaluating each injury individually, considering factors like severity, location, and timing before deciding whether ice application will help or hinder recovery.
In conclusion, while ice therapy remains a valuable tool in injury management, its application should be strategic and informed. Understanding why ice helps when an athlete is injured, as well as recognizing its limitations, allows for more effective and safer treatment protocols. As research continues to evolve, so too will our approaches to using cold therapy in injury recovery and pain management.
References
[1] - https://www.verywellhealth.com/how-long-should-you-ice-an-injury-2696108
[2] - https://nortonhealthcare.com/news/how-long-to-ice-an-injury/
[3] - https://health.clevelandclinic.org/how-long-to-ice-an-injury
[4] - https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/cryotherapy-cold-therapy-for-pain-management
[5] - https://www.orthocarolina.com/media/ice-vs-heat-what-should-i-use-when
[6] - https://advance.muschealth.org/library/2022/september/ice-on-acute-injuries
[7] - https://www.mcrehabilitation.com/blog/the-myth-about-icing-an-injury
[8] - https://pmc.ncbi.nlm.nih.gov/articles/PMC8173427/
[9] - https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/ice-packs-vs-warm-compresses-for-pain
[10] - https://www.verywellhealth.com/how-to-ice-an-injury-2548842
[11] - https://www.boystownhospital.org/knowledge-center/injury-use-ice-heat
[12] - https://www.scoi.com/patient-resources/education/articles/should-you-ice-or-heat-injury
[13] - https://emedicine.medscape.com/article/1833084-overview
[14] - https://www.health.com/ice-baths-8404207
[15] - https://herlongsportspt.com/blog/your-guide-to-icing-and-heating-for-injuries/
[16] - https://journal.parker.edu/article/120141-the-efficacy-of-icing-for-injuries-and-recovery-a-clinical-commentary
[17] - https://www.hackensackmeridianhealth.org/en/healthu/2019/11/14/strains-sprains-chronic-pain-when-to-apply-ice-versus-heat-packs
[18] - https://www.uclahealth.org/medical-services/spine/treatments-programs/nonsurgical-treatment/ice-therapy
[19] - https://www.webmd.com/first-aid/rice-method-injuries