When to Use Hot or Cold Compress: A Doctor's Guide to Pain Relief
Whether you've twisted an ankle or woken up with a stiff neck, knowing when to use hot vs cold compress can make the difference between relief and prolonged discomfort. Many people reach for the wrong temperature therapy, potentially making their pain worse instead of better.
Pain relief doesn't always require medication. Simple hot and cold therapy, along with modern solutions like icy hot cream, heating and cooling balms, and cbd topicals, can effectively manage different types of pain. However, the key lies in understanding which temperature to use and when.
This doctor-approved guide will help you make the right choice for your specific pain condition, explain proper application techniques, and highlight common mistakes to avoid when using hot and cold therapy for pain relief.
Understanding Pain Types and Temperature Effects
Pain manifests differently in each person's body, with varying thresholds for what feels uncomfortable or unbearable. Research shows approximately 50 million adults in the United States experience chronic pain, resulting in economic costs exceeding $600 billion annually [1].
Acute vs. chronic pain responses
Acute pain appears suddenly and typically resolves within six months once the underlying cause is addressed [1]. Specifically, acute pain serves as an immediate warning signal, prompting quick action. Conversely, chronic pain persists beyond six months, continuing even after the initial injury heals [1].
How temperature affects blood flow
Hot and cold therapy fundamentally alters blood flow patterns in the body. Cold application triggers vasoconstriction, reducing blood flow to the affected area [2]. Subsequently, removing the cold source causes vasodilation, as blood vessels expand to compensate, bringing nutrients to help injured tissues heal [2].
Heat therapy, primarily, works by dilating blood vessels and increasing circulation [2]. Furthermore, this improved blood flow helps eliminate lactic acid buildup that occurs after certain types of exercise [2].
Pain signals and nerve responses
Temperature significantly influences how nerves transmit pain signals. Studies demonstrate that cold therapy can reduce sensory nerve conduction velocity by up to 22.6 meters per second [3]. Additionally, motor nerve conduction velocity decreases by up to 8.3 meters per second during cold water immersion [3].
The body's autonomic nervous system responds differently to various temperature levels. Research indicates that a person's perception of pain more strongly influences the body's automatic response than the actual temperature itself [4]. Consequently, two people exposed to the same temperature might experience vastly different levels of discomfort based on their individual pain thresholds [4].
Hot and cold therapy affects pain through multiple mechanisms. Cold numbs pain by decreasing tissue metabolism and blocking nerve impulses [5]. Heat therapy, alternatively, activates heat-sensitive calcium channels, which can alter pain perception by increasing intracellular calcium levels [5].
When to Choose Cold Therapy
Cold therapy stands out as a powerful first-line defense against acute injuries. The science behind cold therapy, also known as cryotherapy or cryokinetics, centers on its ability to constrict blood vessels and decrease circulation to specific areas [2].
Fresh injuries and swelling
Applying cold therapy immediately after an injury proves most effective [2]. The cold constricts blood vessels, primarily reducing blood flow to the affected area. This action helps minimize swelling, particularly around joints and tendons [2]. Moreover, cold therapy should be applied for 10 to 15 minutes, never exceeding 20 minutes at a time to prevent tissue damage [2].
Cold therapy works best for:
-
Sports injuries like sprains and strains
-
Runner's knee and tendonitis
-
Post-surgery swelling
-
Pain under casts or splints [6]
-
Muscle strains and joint pain
Research shows that cold treatment reduces prostaglandin E2 production in tendons - an inflammatory molecule responsible for pain and increased blood flow [7]. Accordingly, this reduction helps decrease both pain and swelling effectively.
Inflammation-related pain
For acute soft-tissue injuries, cold therapy serves as an immediate treatment to induce pain relief [7]. The cold temperature numbs the affected area, reducing both pain and tenderness [8]. Therefore, this approach proves particularly beneficial when swelling becomes a limiting factor in recovery [7].
Cold therapy should only be used for the first 48-72 hours following an injury [9]. This timing aligns with the body's natural inflammatory response. Particularly for athletes dealing with overuse injuries, applying ice after activity helps control inflammation [9].
A crucial safety note: never apply frozen items directly to skin, as this can damage tissues [2]. Additionally, individuals with poor circulation should avoid cold therapy [2]. For optimal results, ice the affected area several times throughout the day, maintaining consistent intervals between applications [2].
The effectiveness of cold therapy stems from its triple action: easing pain through numbing, reducing swelling through vasoconstriction, and decreasing bleeding in the affected tissues [8]. Nevertheless, while cold therapy effectively limits edema, it does not necessarily speed up the overall recovery process [7].
When considering ice or heat for muscle spasm, it's important to note that ice for muscle spasm can be beneficial in certain cases, especially when the spasm is accompanied by inflammation or swelling.
When to Use Heat Therapy
Heat therapy stands as a powerful ally against persistent muscle pain and chronic conditions. The science behind hot therapy centers on its ability to dilate blood vessels, boosting circulation to affected areas [10].
Muscle stiffness and tension
Heat therapy for pain primarily targets areas affected by stiffness and muscle tension. Notably, neck, back, and shoulder regions respond particularly well to hot therapy application [4]. The increased blood flow delivers more oxygen and nutrients to injured tissues, simultaneously promoting healing and reducing discomfort [1].
For muscle recovery, heat therapy offers several key benefits:
-
Speeds up healing through enhanced blood circulation
-
Reduces muscle spasms and related pain
-
Increases flexibility and range of motion
-
Prepares muscles for physical activity
Research demonstrates that heat application before exercise can help limber up muscles and improve performance [11]. Essentially, a 15-20 minute heat session proves sufficient for minor stiffness, though moderate-to-severe pain might benefit from longer treatments lasting 30 minutes to two hours [10].
Chronic pain conditions
Heat therapy undoubtedly shines in managing long-term pain conditions. Studies show that patients with arthritis and fibromyalgia who participated in warm water exercise programs experienced up to 40% less pain [12]. The warmth generally helps loosen stiff joints and promotes better mobility.
Heat therapy works exceptionally well for:
-
Lower back pain through increased blood flow and muscle relaxation [1]
-
Arthritis-related joint stiffness
-
Fibromyalgia symptoms
-
Post-exercise muscle soreness [13]
-
Headaches, when applied to the neck and shoulders
Research indicates that heat therapy can reduce reliance on pain medications, offering a cost-effective alternative with minimal side effects [1]. A morning routine incorporating heat therapy, such as a warm bath or using heating pads, can significantly decrease morning stiffness and improve daily mobility [12].
For optimal results, apply heat for 15 minutes with at least 30 minutes between sessions [14]. Heat therapy proves most beneficial when the pain source is at least several days old, as applying heat too soon after an injury might increase inflammation [15]. The warmth promotes healing by increasing blood flow to the affected area, delivering essential nutrients and oxygen while helping remove inflammatory factors [13].
Proper Application Techniques
Proper application of hot and cold therapy requires attention to specific guidelines and safety protocols. Research shows that incorrect application can diminish therapeutic benefits or potentially cause harm.
Duration guidelines
First and foremost, cold therapy should be limited to 10-15 minutes per session, never exceeding 20 minutes [2]. After each cold application, allow at least 40-60 minutes between sessions [16]. As shown above, this timing prevents the body's negative response of dilating vessels, which could increase inflammation [16].
For heat therapy, minor stiffness typically responds to 15-20 minute sessions [2]. In fact, moderate to severe pain might benefit from extended heat treatments lasting between 30 minutes and two hours [2]. Primarily, heat therapy sessions should not exceed 45-60 minutes without a one-hour recovery period [17].
Temperature safety
Safety measures are crucial for preventing tissue damage. Key precautions include:
-
Never apply ice packs or heating pads directly to skin - always use a thin barrier like a towel [16]
-
Stop treatment immediately if increased swelling occurs [2]
-
Avoid using hot and cold therapy while sleeping [3]
-
Do not apply on broken skin or areas with poor circulation [3]
-
Allow skin to return to normal temperature between applications [5]
Important to realize, the therapeutic range for heat application falls between 40-45°C (104-113.9°F) [17]. Coupled with proper insulation, this range ensures effective treatment without risking tissue damage [16].
Compression levels
Research demonstrates that compression enhances the effectiveness of cold therapy [18]. After all, studies indicate that ice application with compression leads to significantly lower interface temperatures (mean 6.1°C) compared to ice without compression (mean 8.1°C) [18].
The optimal compression level varies based on individual tolerance. While there's no universal standard for compression force [18], applying firm pressure without causing discomfort proves most effective [18]. Notably, higher compression levels achieve minimum temperatures more quickly - 5 minutes with 44 mmHg compression versus 9 minutes without compression [18].
For best results, secure cold or hot packs with elastic bandaging that provides moderate compression [19]. This combination maximizes the depth of temperature change and speeds up lymph evacuation [19]. Research confirms that cold compression therapy works most effectively when applied immediately after injury or surgery [19].
Common Mistakes to Avoid
Making mistakes with hot and cold therapy can worsen injuries and delay healing. Understanding common errors helps prevent complications and ensures effective pain management.
Wrong temperature choice
Selecting incorrect temperature therapy primarily leads to prolonged recovery. Research shows that applying heat to fresh injuries increases inflammation and pain [20]. First and foremost, using ice on muscle spasms or tension can worsen the condition [20].
High-risk conditions requiring careful temperature selection include:
Despite common beliefs, higher temperatures do not guarantee better results [21]. In contrast, excessive heat can trigger skin conditions and increase inflammation [9]. Above all, patients with cardiovascular problems need gradual temperature reduction after heat therapy [9].
Incorrect timing
Timing mistakes often stem from overuse or premature application. Studies indicate that excessive ice usage can delay healing [22]. As a result, experts recommend leaving 20-40 minutes between sessions [22].
Heat therapy should not be used within the first 48 hours after injury [23]. Additionally, prolonged heat application risks developing erythema ab igne - a web-like rash pattern that may require biopsy for pre-cancerous cell testing [9].
Research demonstrates that cold therapy exceeding 20 minutes triggers reactive vasodilation [14]. Hence, the body attempts to increase blood flow to the treated area, potentially worsening inflammation [14]. The ideal protocol maintains 20 minutes on and at least 30 minutes off for ice therapy [14].
Direct skin contact risks
Direct skin exposure to hot and cold therapy poses significant risks. Applying frozen items directly to skin can cause ice burns and tissue damage [24]. Alternatively, direct contact with heating devices risks contact burns and skin reactions [9].
Medical studies confirm that skin integrity checks are essential before any heat application [21]. Furthermore, compromised circulation in the affected area contraindicates both heat and cold therapy [8]. For diabetic patients or those with peripheral vascular disease, temperature therapy requires extra precaution due to altered sensitivity [21].
Proper barriers between skin and temperature sources prevent complications. Research supports using thin towels or clothing layers to protect against both ice burns and heat-related injuries [25]. For optimal safety, maintain consistent monitoring during treatment and stop immediately if experiencing increased pain or discomfort [26].
Patients with certain pre-existing conditions face heightened risks from improper temperature therapy. Those with diabetes, dermatitis, vascular diseases, deep vein thrombosis, or multiple sclerosis should consult healthcare providers before starting any hot and cold therapy regimen [27]. Excessive alcohol use or dehydration during heat therapy may lead to unconsciousness, resulting in serious burns and potential kidney damage [9].
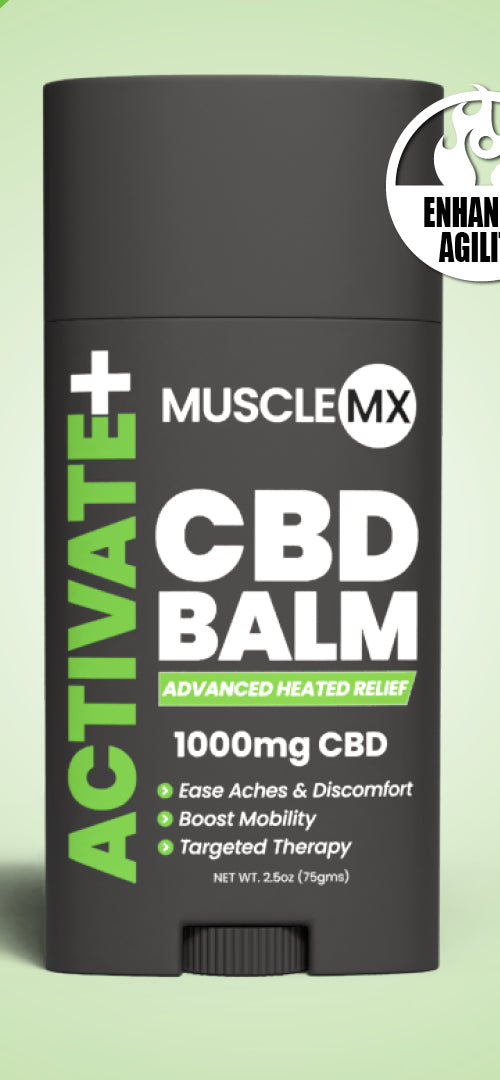
Muscle MX Activate and Recovery CBD balms offer a dual approach to pain management through safe hot and cold therapy. The Activate balm is designed to warm the muscles, enhancing blood flow and preparing the body for physical activity, which can help prevent injuries and reduce pain. On the other hand, the Recovery balm provides a cooling sensation that soothes inflammation and eases muscle tension post-exercise. Both balms are infused with CBD, known for its anti-inflammatory properties, which can further aid in reducing pain and promoting recovery. This combination of hot and cold therapy, along with the benefits of CBD, makes Muscle MX balms a versatile and effective option for managing pain safely.
Conclusion
Hot and cold therapy stands as a powerful tool for pain management when applied correctly. Understanding whether to use heat or cold makes the difference between relief and potential complications. Cold therapy excels at managing acute injuries and inflammation during the first 48-72 hours, while heat therapy works best for chronic pain and muscle stiffness.
Proper application remains crucial for effective results. Following recommended duration guidelines - 10-15 minutes for cold therapy and 15-20 minutes for heat therapy - helps maximize benefits while preventing tissue damage. Safety precautions, such as using protective barriers and maintaining appropriate intervals between sessions, protect against complications.
Remember that hot and cold therapy might not suit everyone. People with diabetes, circulation problems, or certain medical conditions should consult healthcare providers before starting any temperature therapy for chronic pain regimen. Careful attention to timing, temperature choice, and application methods ensures safe and effective pain relief without medication.
The benefits of hot and cold therapy are numerous when used correctly. From reducing inflammation with cold compresses to easing muscle tension with heating pads or hot water bottles, these methods offer versatile solutions for various pain conditions. Contrast therapy, which alternates between hot and cold treatments, can be particularly effective for certain injuries and chronic pain conditions.
Whether you're dealing with acute injuries that require the RICE treatment (Rest, Ice, Compression, Elevation) or chronic conditions that benefit from the soothing warmth of thermotherapy, understanding how does heat therapy work and what does hot cold therapy do can significantly improve your pain management strategy. By incorporating these techniques into your routine, you can harness the power of temperature to promote healing, reduce pain, and enhance overall well-being.
References
[1] - https://www.spine-health.com/treatment/heat-therapy-cold-therapy/benefits-heat-therapy-lower-back-pain
[2] - https://www.healthline.com/health/chronic-pain/treating-pain-with-heat-and-cold
[3] - https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.using-cold-and-heat-therapies.acn6587
[4] - https://uspainfoundation.org/news/the-benefits-of-heat-and-cold-therapy-for-chronic-pain/
[5] - https://www.webmd.com/pain-management/when-use-heat-ice
[6] - https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=85&contentid=p00918
[7] - https://pmc.ncbi.nlm.nih.gov/articles/PMC8173427/
[8] - https://www.mdd.gov.hk/filemanager/common/information-publication/hot_and_cold_eng_20200121_v6_with_photo.pdf
[9] - https://www.spine-health.com/treatment/heat-therapy-cold-therapy/potential-risks-and-contraindications-heat-therapy
[10] - https://www.aoaortho.com/heat-and-cold-therapy-for-pain-management/
[11] - https://www.piedmont.org/living-real-change/when-to-treat-pain-with-ice-vs-heat
[12] - https://www.arthritis.org/health-wellness/healthy-living/managing-pain/pain-relief-solutions/heat-therapy-helps-relax-stiff-joints
[13] - https://pmc.ncbi.nlm.nih.gov/articles/PMC8862647/
[14] - https://www.orthocarolina.com/media/ice-vs-heat-what-should-i-use-when
[15] - https://www.beaumont.org/health-wellness/blogs/when-to-use-ice-and-when-to-use-heat-for-aches-and-pains
[16] - https://www.hackensackmeridianhealth.org/en/healthu/2019/11/14/strains-sprains-chronic-pain-when-to-apply-ice-versus-heat-packs
[17] - https://www.cardinalhealth.com/content/dam/corp/web/documents/whitepaper/cardinal-health-localized-temperature-therapy White Paper.pdf
[18] - https://www.sciencedirect.com/science/article/abs/pii/S0031940606000824
[19] - https://pmc.ncbi.nlm.nih.gov/articles/PMC3781860/
[20] - https://www.emoryhealthcare.org/stories/ortho/use-heat-ice-treat-injury
[21] - https://pmc.ncbi.nlm.nih.gov/articles/PMC9845456/
[22] - https://www.texashealth.org/Health-and-Wellness/Sports-Medicine/Ice-vs-Heat-How-to-Decide-Which-is-Best-for-Your-Injury
[23] - https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/ice-packs-vs-warm-compresses-for-pain
[24] - https://www.medicalnewstoday.com/articles/322606
[25] - https://www.healthline.com/health/ice-burn
[26] - https://www.vivehealth.com/blogs/resources/alternating-hot-and-cold-therapy?srsltid=AfmBOorGPetXxilHnN73C7HH9PWTYFQztccb1dZmqnQ47uXWoHaNZ1eq
[27] - https://www.unchealthappalachian.org/blog/2024/heat-vs-cold-what-works-better/