The Strongest Over The Counter Painkillers: What Pharmacists Won't Tell You
Pain strikes when you least expect it, and reaching for the strongest over the counter painkiller seems like the obvious solution. However, what many people don't realize is that the effectiveness of these medications depends on far more than just their labeled strength. While standard over the counter painkillers promise quick relief, their actual power can vary dramatically based on factors that pharmacists rarely discuss with customers. In fact, something as simple as when you take the medication or what you've eaten can make a significant difference in how well it works.
Let's explore what really determines painkiller effectiveness, the strongest options available, and smart strategies to maximize their relief potential. We'll also examine why some people are turning to alternatives like CBD for pain management when traditional painkillers fall short.
Understanding Pain Relief Strength
Different painkillers available at pharmacies work through distinct mechanisms to provide relief. Understanding these differences helps explain their varying levels of effectiveness.
How painkillers are ranked
Medical researchers rank over-the-counter painkillers using two primary measurements. The first is the Number Needed to Treat (NNT), where lower numbers indicate greater effectiveness. The second is the success rate, which measures the percentage of people who experience significant pain relief .[1]
Based on these measurements, combinations of ibuprofen plus acetaminophen rank highest with NNT values below 2 and success rates reaching nearly 70% . Furthermore, fast-acting ibuprofen formulations and ibuprofen combined with caffeine show success rates above 50% .[1][1]
What makes one stronger
The strength of a painkiller primarily depends on its active ingredients and mechanism of action. NSAIDs, including ibuprofen and naproxen, work by blocking specific enzymes (COX-1 and COX-2) that produce pain-causing chemicals . Alternatively, acetaminophen functions by raising the body's pain threshold .[2][3]
Several factors determine a painkiller's potency:
-
Active Ingredients: Naproxen stands out as the most potent anti-inflammatory option available without prescription[3]
-
Combination Effects: Taking ibuprofen with acetaminophen can provide stronger relief than either medication alone[1]
-
Formulation Type: Fast-acting versions of medications often show higher success rates compared to standard formulations[1]
Notably, the effectiveness of these medications varies based on the type of pain being treated. NSAIDs excel at reducing inflammation and swelling from conditions like arthritis , whereas acetaminophen proves particularly effective for headaches and fever reduction .[4][3]
Understanding these differences becomes crucial since what works best for one person might not be as effective for another . Additionally, the timing and method of taking these medications significantly influence their effectiveness - a factor often overlooked by consumers seeking quick relief.[4]
The Strongest OTC Options Available
Among available pain relievers, certain medications stand out for their exceptional strength and effectiveness. Understanding these options helps make informed choices for pain management, including alternatives like CBD for chronic pain.
Naproxen: The power player
Naproxen stands as the strongest non-prescription NSAID available . This medication delivers longer-lasting relief, requiring fewer doses throughout the day . A single dose provides pain relief for 8-12 hours, essentially doubling the duration of other common pain relievers .[5][5][5]
Primarily used for sprains, sunburns, and arthritis conditions, naproxen comes in 220mg tablets . Nevertheless, adults over 65 should exercise caution with naproxen due to increased risks of side effects .[5][5]
Maximum strength combinations
Research shows that combining different types of pain relievers can enhance their effectiveness . One particularly potent combination pairs acetaminophen with ibuprofen. This duo provides superior pain relief compared to using either medication alone .[6][6]
Key benefits of combination therapy include:
-
Enhanced pain relief without increasing individual drug doses
-
Simplified dosing schedules
-
Better overall effectiveness than single-drug approaches[6]
Modern formulations now offer these combinations in single tablets, making them more convenient for users. For instance, some products combine 500mg acetaminophen with 150mg ibuprofen .[6]
Time-release formulations
Time-release medications represent a significant advancement in pain management. These formulations utilize bi-layer technology to provide both immediate and extended relief . For example, certain acetaminophen products feature two distinct layers - one that dissolves quickly for fast action, followed by a second layer that provides up to 8 hours of continuous relief .[7][7]
The extended-release design offers several advantages:
-
Consistent pain relief throughout the day
-
Reduced frequency of dosing
-
Better compliance with treatment schedules
Specifically, these formulations excel at managing chronic conditions like arthritis while maintaining effectiveness for other types of pain, including headaches, muscle aches, and menstrual cramps .[7]
Hidden Factors That Affect Painkiller Power
Most people assume that taking the strongest over the counter painkiller guarantees relief, yet surprising factors can significantly alter their effectiveness. Research reveals that both meal timing and the hour of day play crucial roles in how well these medications work.
Empty vs full stomach impact
Contrary to common advice, taking painkillers with food might actually reduce their effectiveness . Studies show that food typically delays absorption for common painkillers, with absorption times increasing by 1.3 to 2.8 times compared to taking them on an empty stomach .[8][8]
The impact becomes even more pronounced when examining maximum concentration levels. Research indicates that taking painkillers with food can reduce their peak effectiveness to just 44-85% of what's achieved on an empty stomach . This reduction occurs primarily because:[8]
-
Food delays delivery to the intestine, the main absorption site[9]
-
Decreased gastric movement affects drug dissolution[9]
-
Altered blood flow patterns impact absorption rates[9]
Consequently, for acute pain relief, taking medications on an empty stomach often proves more effective . Moreover, research has debunked the myth that food prevents stomach irritation - studies show no convincing evidence that taking occasional over-the-counter NSAIDs with food prevents side effects .[10][10]
Time of day differences
The body's natural 24-hour rhythm substantially influences painkiller effectiveness . Scientists have discovered that medications can produce different responses depending on when they're taken, with some fascinating patterns emerging:[4]
Pain sensitivity naturally fluctuates throughout the day, showing lowest levels between 1 PM and 11 PM . Subsequently, this timing coincides with enhanced painkiller efficacy during afternoon and early evening hours .[4][4]
Research has uncovered that skin sensitivity to pain peaks at 6 AM and reaches its lowest point at 6 PM . Similarly, studies examining labor pain management found that women receiving pain medication between noon and 6 PM experienced 27% longer relief compared to those treated between 8 PM and 2 AM .[4][11]
These variations stem from the body's circadian rhythm affecting multiple factors:
-
Drug metabolism rates change throughout the day[12]
-
Pain receptor sensitivity fluctuates[4]
-
Hormone levels vary, impacting drug effectiveness[4]
Understanding these hidden factors becomes crucial for maximizing painkiller effectiveness. Primarily, the timing of administration can mean the difference between optimal relief and subpar results. This knowledge proves particularly valuable when dealing with scheduled doses or managing chronic pain conditions.
Smart Timing Strategies
Maximizing the effectiveness of pain relief requires strategic timing and careful planning. Research shows that understanding medication onset times and peak effectiveness windows can dramatically improve pain management outcomes.
Peak effectiveness windows
Timing plays a crucial role in pain relief effectiveness. According to medical research, acetaminophen typically takes 30-45 minutes to start working and reaches peak effectiveness within 0.5-1 hours . In contrast, ibuprofen demonstrates peak anti-inflammatory effects within 1-2 weeks of routine administration .[2][13]
For optimal results, consider these peak effectiveness periods:
-
Naproxen reaches full anti-inflammatory potential within 2-4 weeks of consistent use[13]
-
Ibuprofen shows initial effects within 30-60 minutes[13]
-
Acetaminophen maintains effectiveness for 4-6 hours per dose[2]
Duration planning
Proper duration planning ensures consistent pain relief throughout the day. Rather than waiting for pain to return, scheduling doses based on medication duration proves more effective. For instance, naproxen offers extended coverage, lasting 8-12 hours per dose .[14]
The ideal approach involves using the lowest effective dose over the shortest necessary period . Accordingly, adults should limit acetaminophen to 3,000 mg daily , whereas ibuprofen should not exceed 1,200 mg in 24 hours .[15][2][16]
Avoiding gaps in coverage
One effective strategy for maintaining consistent pain relief involves alternating different types of medications. Indeed, research supports taking ibuprofen and acetaminophen in a staggered pattern . This method allows for one pill every 2-4 hours while staying within safe daily limits.[1]
A recommended four-hour schedule might include:
-
Ibuprofen at 8 AM
-
Acetaminophen at noon
-
Ibuprofen at 4 PM
-
Acetaminophen at 8 PM[1]
Certainly, if pain persists after an hour, switching to a different type of pain reliever proves more effective than repeating the same medication . Generally, experts recommend waiting 4-6 hours between doses of the same medication .[17][17]
Finally, research indicates that taking painkillers before exercising remains safe , although timing should align with peak effectiveness windows for optimal results. Nonetheless, if daily pain relief becomes necessary for two weeks or longer, consulting a healthcare provider becomes essential .[2][15]
Common Mistakes That Reduce Effectiveness
Taking over-the-counter painkillers might seem straightforward, yet research reveals that common mistakes can drastically reduce their effectiveness. Understanding these errors helps ensure optimal pain relief while maintaining safety.
Wrong combinations
Mixing medications incorrectly poses serious risks. Studies show many patients unknowingly take dangerous combinations of medications, primarily because they don't read labels carefully .[18]
Some hazardous combinations include:
-
Multiple NSAIDs together, which increases bleeding risk[18]
-
Acetaminophen with multi-symptom cold medications, risking liver damage[19]
-
NSAIDs with blood pressure medications, which can reduce effectiveness[18]
-
Anticoagulants with NSAIDs, leading to increased bleeding risk[18]
First, check active ingredients in all medications you're taking. Many prescription pain medicines contain acetaminophen or NSAIDs . Hence, combining them with similar over-the-counter medications puts you at risk for overdosing .[20][20]
Poor timing choices
Timing errors can significantly impact medication effectiveness. Research indicates that NSAIDs block aspirin's blood-thinning benefits when taken incorrectly . Therefore, if you take daily aspirin for heart health, wait at least 30 minutes after your aspirin dose before taking an NSAID .[3][3]
Likewise, studies reveal that NSAIDs can affect blood pressure. The impact is strongest in people already taking blood pressure medication . Still, evidence suggests these medications may affect people with normal blood pressure as well .[3][3]
Storage errors
Proper storage proves crucial for maintaining medication effectiveness. The Environmental Protection Agency urges storing medicines in locked cabinets, closets, or safes . Despite widespread availability, many households fail to implement safe storage methods .[21][21]
Key storage considerations include:
-
Temperature control
-
Protection from moisture
-
Original container maintenance
-
Child-resistant packaging
-
Regular expiration date checks
Primarily, medications should remain in their original containers with child-resistant caps . Regardless of convenience, avoid leaving medications on counters or in easily accessible locations .[22][22]
Research indicates that approximately 40% of medications sold end up unused . Yet, improper storage can lead to deterioration or accidental use of expired products . As well as affecting medication potency, poor storage practices may result in:[23][5]
Dr. Charles Vega, clinical professor at the University of California at Irvine, emphasizes that despite their over-the-counter status, these medications demand serious attention . "These are real medicines with real consequences," he states .[24][24]
Alternatively, consider implementing a medication tracking system. This helps monitor expiration dates and prevents unintended use of deteriorated products. Furthermore, proper disposal of unused medications through designated programs prevents misuse and environmental contamination .[22]
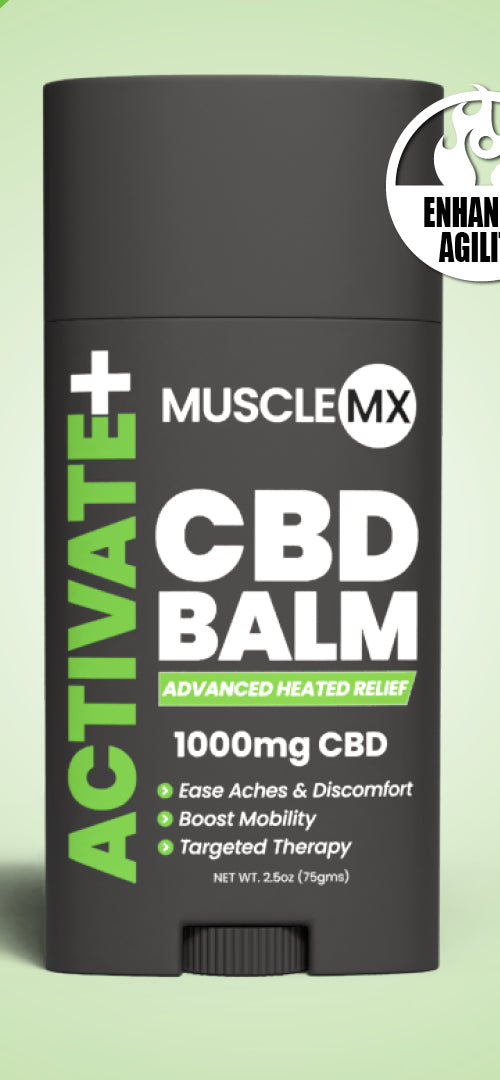
CBD and Cannabis for Pain Relief: A Growing Alternative
As traditional painkillers face scrutiny for potential side effects and addiction risks, many are turning to CBD for pain management. Cannabidiol (CBD), a non-psychoactive compound found in cannabis, has gained attention for its potential analgesic effects and role in pain mechanisms.
How CBD helps with pain
CBD interacts with the body's endocannabinoid system, which plays a crucial role in regulating pain, mood, and sleep. By modulating cannabinoid receptors, particularly CB1 and CB2 receptors, CBD may help reduce pain and inflammation. Research suggests that CBD's impact on pain signaling and stress response could contribute to its analgesic effects.
Clinical trials exploring CBD for chronic pain have shown promising results. Studies indicate that CBD may help with various types of pain, including neuropathic pain and nociplastic pain. Additionally, CBD's potential for anxiety reduction and sleep improvement may indirectly benefit those suffering from chronic pain conditions.
CBD vs THC for pain relief
While both CBD and THC (tetrahydrocannabinol) are cannabinoids found in cannabis, they interact with the body differently. THC is known for its psychoactive effects and pain-relieving properties, while CBD offers potential pain relief without the "high" associated with THC.
Some research suggests that combining CBD and THC may provide enhanced pain relief compared to using either compound alone. This synergistic effect, often referred to as the "entourage effect," is the basis for many cannabis-based medicines. However, the optimal ratio of CBD to THC for pain management may vary depending on the individual and the type of pain being treated.
Safety and tolerability of CBD
CBD generally demonstrates a favorable safety profile and good tolerability in clinical trials. However, as with any supplement or medication, there are potential side effects and drug interactions to consider. Common side effects of CBD may include fatigue, changes in appetite, and gastrointestinal discomfort.
It's crucial to consult with a healthcare provider before incorporating CBD into your pain management regimen, especially if you're taking other medications. Your doctor can help assess potential drug interactions and determine an appropriate dosage based on your individual needs and medical history.
Legal considerations and quality control
The legality of CBD and cannabis products varies by region, so it's essential to understand local laws before purchasing or using these products. In areas where CBD is legal, it's important to choose high-quality products from reputable sources. Look for products that have been third-party tested and provide clear information about their CBD content and any additional ingredients.
As research on CBD and pain relief continues to evolve, it's likely we'll gain a better understanding of its potential as an opioid alternative and its role in comprehensive pain management strategies. For those seeking new hope in managing chronic pain, CBD represents an intriguing option worth exploring under medical supervision.
Conclusion
Understanding how over-the-counter painkillers work makes a significant difference in pain management success. Though these medications offer relief, their effectiveness depends on proper timing, smart combinations, and careful storage practices.
Research clearly shows that factors like meal timing and time of day affect painkiller performance. Naproxen stands out as the strongest single OTC option, while strategic combinations of acetaminophen and ibuprofen provide enhanced relief when used correctly.
Smart timing strategies paired with proper storage ensure these medications work at their full potential. Avoiding common mistakes such as incorrect combinations or poor timing choices helps maintain both safety and effectiveness.
Remember that even the strongest over-the-counter painkillers require careful consideration. Following evidence-based guidelines for timing, storage, and combinations helps achieve optimal pain relief while maintaining safety. Should pain persist beyond two weeks, consulting a healthcare provider remains the best course of action.
For those seeking alternatives, CBD for chronic pain management represents a growing area of interest. While more research is needed, CBD's potential analgesic effects and impact on quality of life make it an intriguing option for some individuals. As with any pain management strategy, it's crucial to work closely with healthcare professionals to find the most effective and safe approach for your individual needs.
References
[1] - https://www.yalemedicine.org/news/acetaminophen-nsaids-over-the-counter-pain-relievers
[2] - https://medlineplus.gov/ency/article/002123.htm
[3] - https://www.health.harvard.edu/pain/10-things-you-should-know-about-common-pain-relievers
[4] - https://pmc.ncbi.nlm.nih.gov/articles/PMC3004635/
[5] - https://www.ncbi.nlm.nih.gov/books/NBK519065/
[6] - https://pmc.ncbi.nlm.nih.gov/articles/PMC2791549/
[7] - https://www.tylenol.com/products/arthritis/tylenol-8hr-arthritis-pain
[8] - https://pmc.ncbi.nlm.nih.gov/articles/PMC4574824/
[9] - https://pmc.ncbi.nlm.nih.gov/articles/PMC2014238/
[10] - https://www.drugs.com/medical-answers/you-ibuprofen-empty-stomach-3572019/
[11] - https://newsroom.wakehealth.edu/news-releases/2005/09/timing-of-womens-labor-may-determine-effectiveness-of-pain-medication
[12] - https://theconversation.com/timing-matters-for-medications-your-circadian-rhythm-influences-how-well-treatments-work-and-how-much-they-might-harm-you-194906
[13] - https://www.hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/QMP/PainMedicationTable.pdf
[14] - https://www.walgreens.com/health/p2/a/1800002/making-sense-of-otc-pain-relievers-a-decision-guide/2191116
[15] - https://www.health.harvard.edu/pain/know-your-pain-relievers
[16] - https://www.orlandohealth.com/content-hub/tips-for-taking-otc-medications-to-avoid-health-risks/
[17] - https://www.novanthealth.org/healthy-headlines/over-the-counter-pain-relief-what-to-know-when-to-take-it-when-to-be-cautious
[18] - https://pmc.ncbi.nlm.nih.gov/articles/PMC2257951/
[19] - https://www.prevention.com/health/a20471095/dangerous-over-the-counter-medicine-combinations/
[20] - https://www.uhhospitals.org/health-information/health-and-wellness-library/article/adult-diseases-and-conditions-v1/otc-pain-medications-and-their-risks
[21] - https://www.epa.gov/household-medication-disposal/safe-storage-medicines-home
[22] - https://doh.wa.gov/community-and-environment/schools/safety-study-hall/secure-storage-prescription-and-over-counter-drugs
[23] - https://www.agingresearch.org/our-initiatives/safe-medicine-use-storage-and-disposal/
[24] - https://www.menshealth.com/health/g19531729/mistakes-you-make-with-over-the-counter-pain-relievers/